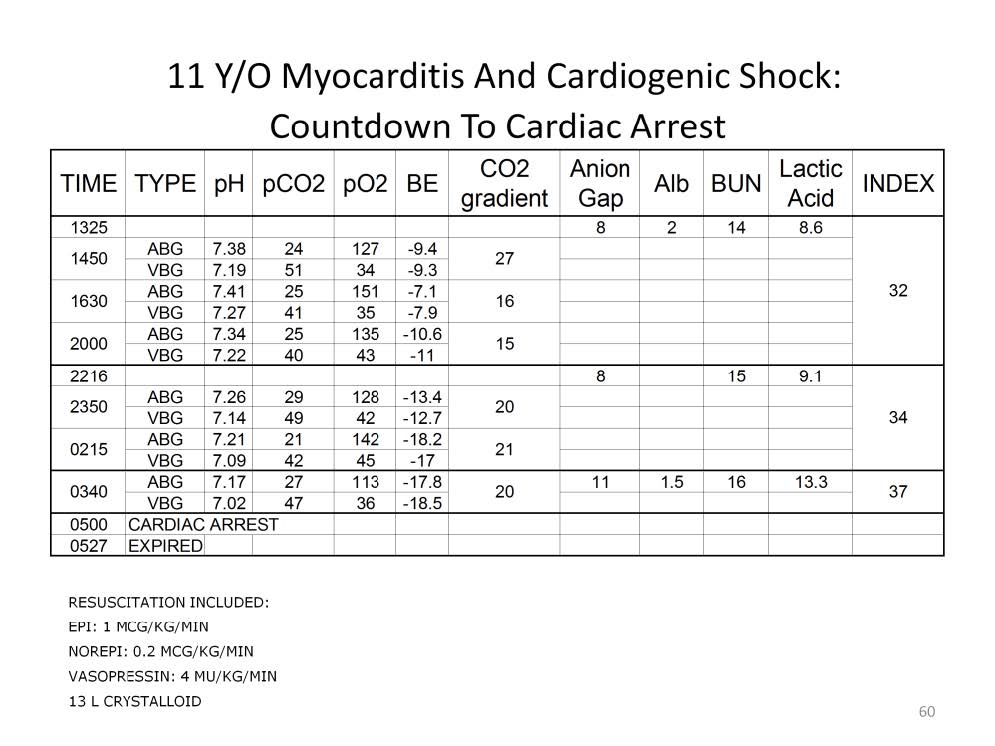
This case is an example of how the Viability Index score would have benefited a patient if it had been utilized. A patient with myocarditis was resuscitated using increasing doses of inotropes, vasopressors and fluid for volume expansion. In the first 6.5 hours, the VI score was 32, at the very bottom of the survival curve. This score alone would not necessarily suggest the need for mechanical cardiopulmonary support if the resuscitation efforts had succeeded. However over the next 7.5 hours the failure of the resuscitation was apparent as the VI score continued to increase. Over the next 2 hours the VI score increased yet again, suggesting the immediate need to implement extracorporeal support. However this was not forth coming. The patient finally arrested and could not be revived after 27 minutes of CPR with ACLS.
If the patient had been placed on extracorporeal support after 2000, the further worsening of the VI score and the cardiac arrest could have been avoided. The patient may or may not have succumbed at a later date to his myocarditis even with ECMO support, but that opportunity to survive was not realized. In addition, placing the patient on ECMO too late at 0340 or even 2350 would have exposed him to the ravages of reperfusion injury aggravated by the pump, further reducing chances for survival.
Timing is an important aspect of implementing extracorporeal support; ‘the earlier the better’ is thought to offer the best chance of survival. However outside of the Viability Index there is no quantifiable standard to determine if extracorporeal support is early enough or too late to save the patient.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.