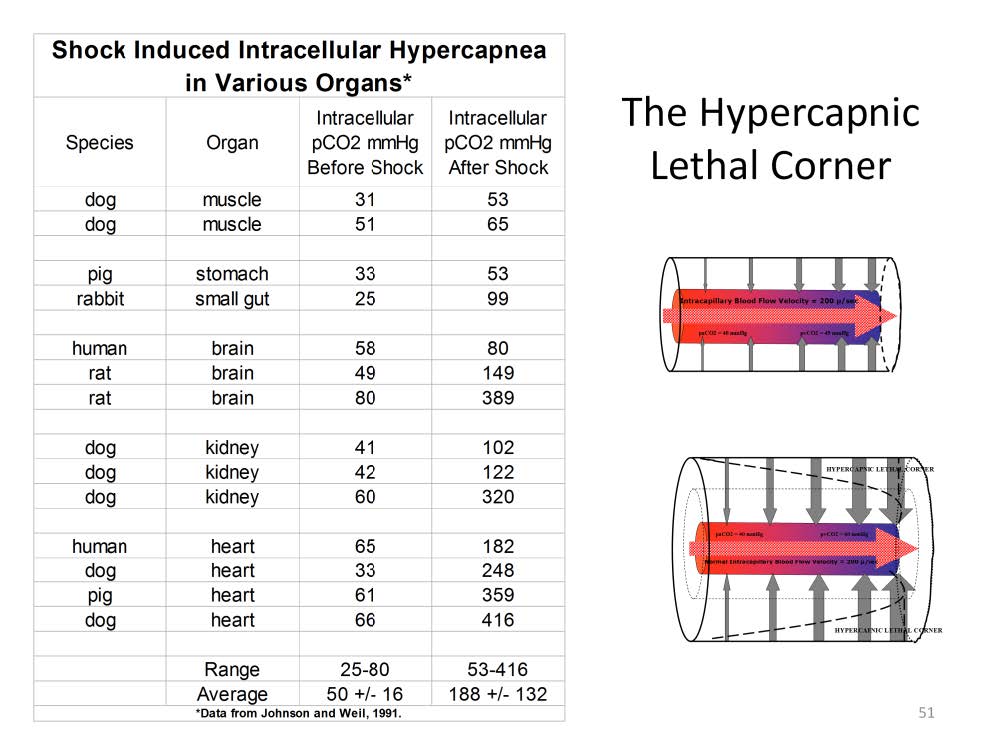
The effect of shock and ischemia on the intracellular pCO2 of various organs. Data complied from Johnson and Weil, 1991.
A meta-analysis published by Johnson and Weil demonstrates the effect of shock on intracellular pCO2. Shock was initiated by hypoxia, reduced blood flow or absolute ischemia in the various experiments. The baseline tissue pCO2 averaged 50 mmHg, followed by a 3.6 fold increase to 188 mmHg during shock. The pCO2 increase is smaller in non-essential muscles, stomach and gut. But, in essential organs such as the brain, kidneys and heart, the intracellular pCO2 increase can be enormous. These experiments give some idea about the magnitude to which the intracellular CO2 concentration can rise during shock. However, this kind of direct assessment of intracellular pCO2 in the clinical setting is impractical. If tissue pCO2 measurements could be made directly on specific organs such as the brain or heart, these would only reflect a local or regional effect. The only practical method to assess intracellular pCO2 is to measure the venoarterial CO2 gradient as suggested by the Krogh model.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.