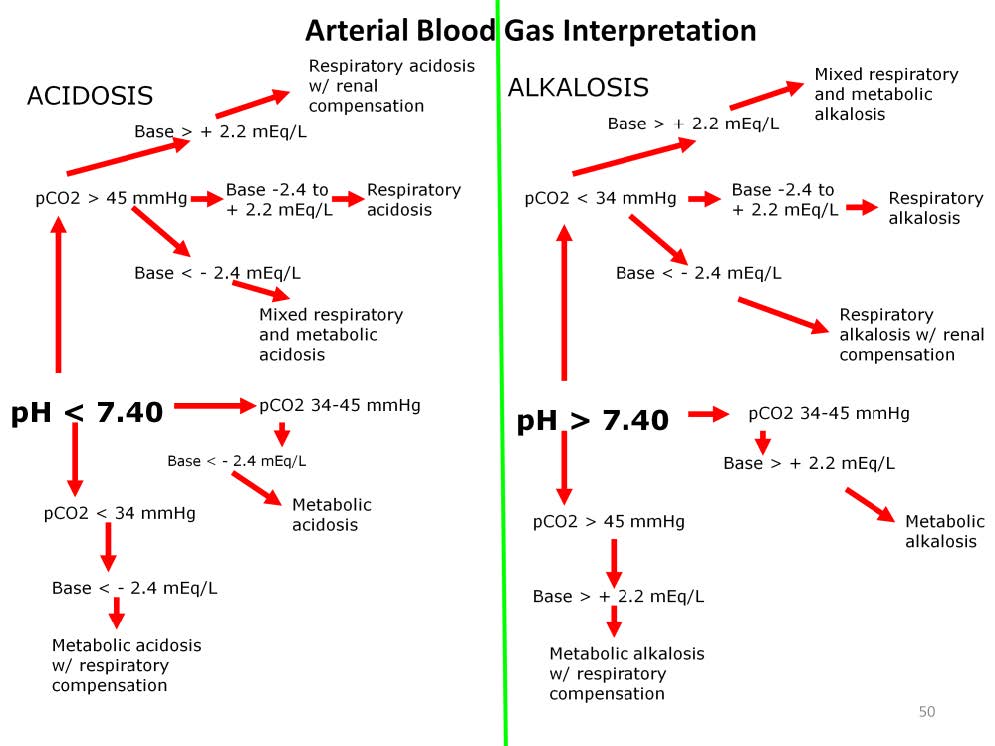
The usual interpretation of the arterial blood gas follows a pattern like that shown above. First the paH is evaluated, then the paCO2. The determination is made if the acidosis or alkalosis is respiratory or metabolic, which are often modified by compensation mechanisms.
The problem for perfusionists and their patients is that this only works for a patient breathing under his own power. Once a patient is placed on a positive pressure ventilator or mechanical cardiopulmonary support, the traditional mode of ABG interpretation is useless because the ventilator or the pump do not allow the patient’s physiology to compensate naturally. In fact, the accepted ABG interpretation under these conditions is worse than useless because it can lead to false reassurance that the patient is stable and has a survivable physiology. The ABG of a patient on a ventilator or extracorporeal support does not provide a reliable measure of tissue pH or pCO2. The only reliable parameter that an ABG provides is the paO2 which reflects the lungs’ ability to exchange oxygen based on changes in the ventilator FiO2. In univentricular patients with mixed systemic and pulmonary blood flow, even this measurement is unreliable.
Arterial blood gas interpretation is the worst dogma in all of critical care and perfusion practice. Without an accompanying central venous blood gas, the ABG cannot be relied upon to assess a patient’s physiology. The APACHE III score relies on both the arterial pH and the arterial pCO2 to determine one of the score’s most important factors. A paH of 7.40 and a pCO2 of 40 mmHg would not add any points to the mortality score. However, a venous blood gas drawn on the same patient at the same time with a pvH of 7.00 and a pvCO2 of 80 mmHg would indicate that the patient is on the verge of imminent death, but not because of the abnormal pH or pCO2. Rather it is the gradient of 40 mmHg between the paCO2 and the pvCO2 which indicates a lethal level of tissue CO2 which will quickly lead to organ dysfunction, hemodynamic instability and cardiac failure and arrest.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.