A p[v-a]CO2 increase is related to the reduction in cardiac output. This suggests a state of shock in the form of poor capillary perfusion, whatever the cause. Because capillary transit time slows down as the cardiac output declines, there is a larger than normal accumulation of CO2 per unit of venous blood. The capillaries are further overloaded as perfused capillary density declines. This results in fewer open capillaries to remove CO2 from the tissues. These factors generate hypercapnea in the venous blood. The relationship is not linear because a change of cardiac output will result in the greatest increase in p[v-a]CO2 (aka DPCO2) in the lowest range of cardiac output. However a simple formula can be used clinically to estimate the cardiac index. In adults the formula is: Cardiac Index = 12.9 / p[v-a]CO2. In infants the formula is: Cardiac Index = 18 / p[v-a]CO2. Infants use a larger constant because of their greater production of CO2/kg.
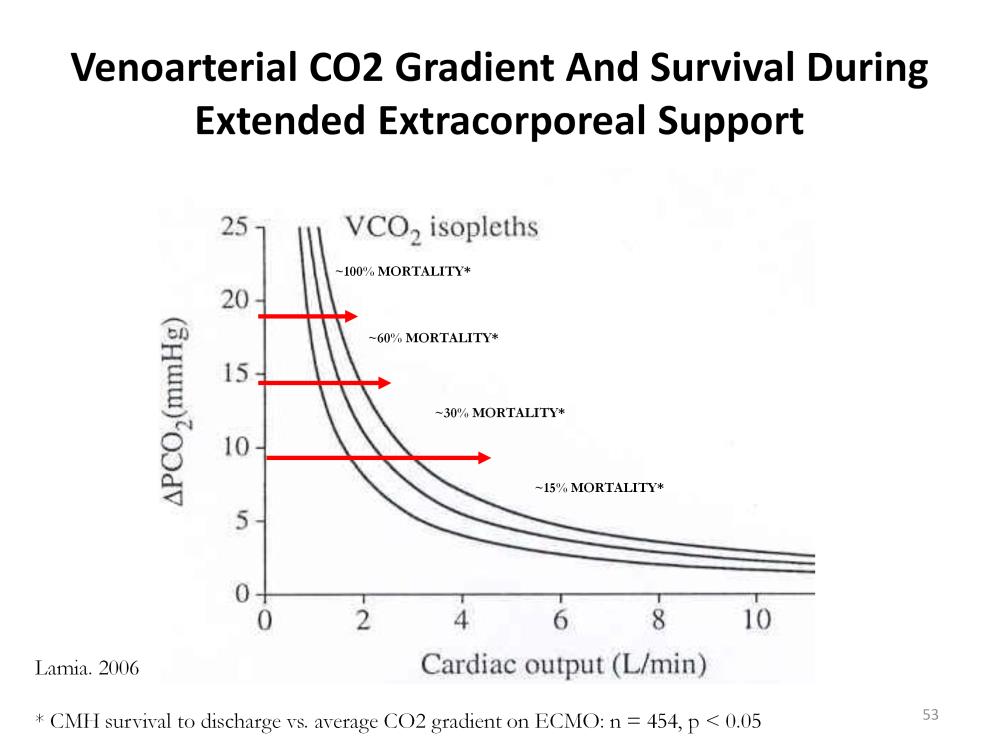
This figure illustrates the lethality of a larger than normal p[v-a]CO2 in 454 ECMO patients. Those patients with an average p[v-a]CO2 over time of less than 10 mmHg have the lowest mortality rate (15%). The mortality rate progressively increases until the average p[v-a]CO2 exceeds 20 mmHg correlating to 100% lethality. Even though these patients are being supported by cardiopulmonary bypass in the form of ECMO, the accumulation of CO2 in the tissues causes lethal complications often independent of the primary diagnosis. For example, a patient with a large p[v-a]CO2 who is suffering from pulmonary hypertension may have an intracranial hemorrhage, renal failure, multiple organ failure or just simply failure to improve.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.