However it is possible to improve the pulmonary and hemodynamic effects of MUF in adults by increasing the osmolarity of the residual CPB circuit volume. MUF increases the oncotic pressure in the infant’s pulmonary artery by hemoconcentrating the residual circuit plasma proteins. However in the adult this could only be accomplished by adding multiple vials of 25% albumin to the residual circuit volume. A better strategy is to increase the osmotic pressure of the pulmonary artery blood. Oncotic pressure is exerted by large, protein molecules. Osmotic pressure is exerted by much smaller but more abundant molecules, usually ions (electrolytes) or sugars. The difference is that the small molecules eventually equilibrate on both sides of the capillary membrane whereas the protein molecules mostly remain within the capillary lumen.
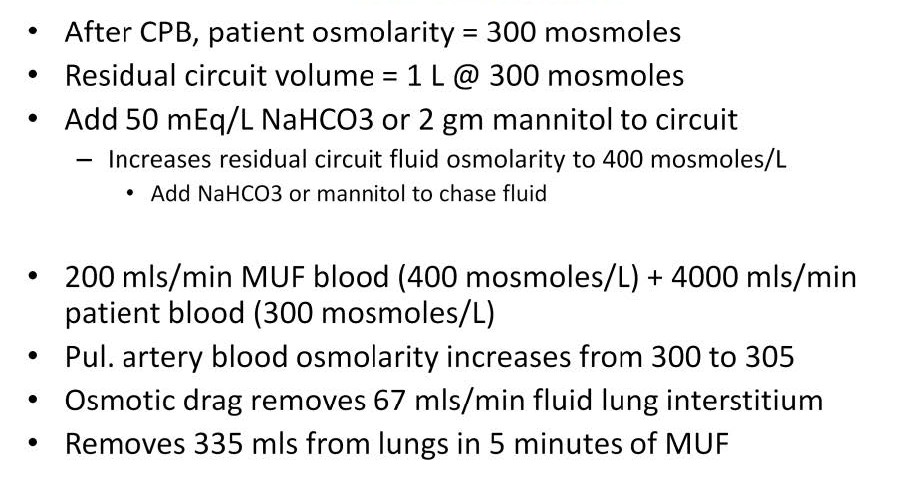
Adding 50 mEq of NaHCO3 or 2 gm of mannitol to each liter of residual circuit volume will increase the osmotic pressure enough so that when the residual circuit volume is mixed 1/20 with the patient’s right atrial circulating blood volume, the osmotic pressure will be high enough to remove excess interstitial pulmonary edema. In the example above, the fluid removed from the lungs by increasing the osmotic pressure of the pulmonary artery blood by only 5 milliosmoles can be calculated at 67 mls/min during 5 minutes at a MUF blood flow of 200 mls/min, for a total of 335 mls removed from the lungs. This method can remove enough lung water to improve hemodynamics and possibly avoid the excessive use of cardiac drugs, diuretics or even mechanical support postoperatively.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.