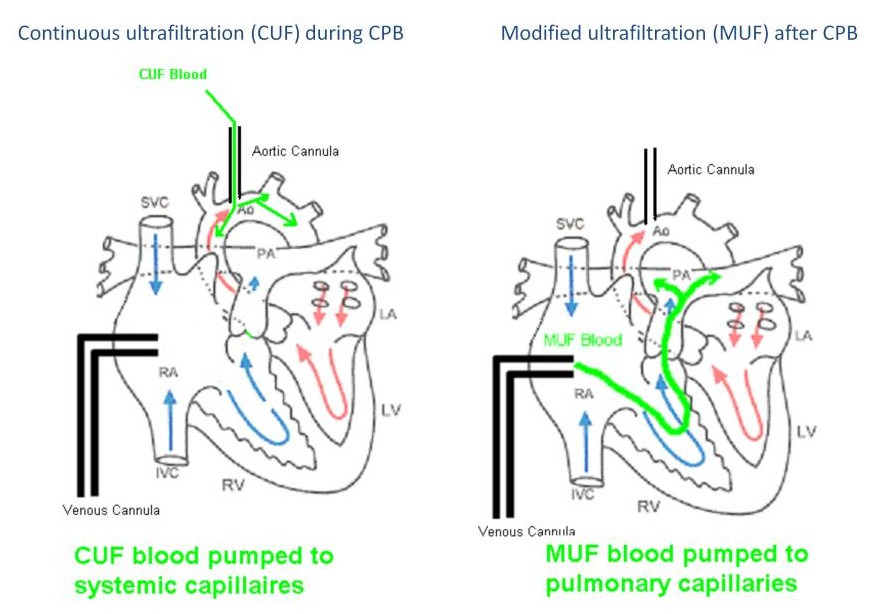
There are two different capillary beds which the perfusionist can target for ultrafiltration. The application of ultrafiltration to each of the target beds gives different physiologic results.
During CPB, continuous ultrafiltration removes fluid from the blood passing through the circuit, concentrating the plasma proteins. Then it is returned to the patient’s systemic circulation via the aorta. The blood entering the aorta has a slightly higher oncotic pressure (colloid osmotic pressure) than the rest of the body. Because large plasma proteins cannot easily pass through the capillary walls, the arterial blood’s higher oncotic pressure tends to pull fluid from the tissues where it is removed by the systemic capillary blood flow, thus reducing systemic organ and peripheral edema. If the ultrafiltration is too aggressive, the patient’s circulating blood volume is reduced too rapidly causing hypovolemia resulting in inadequate perfusion. This necessitates the administration of IV fluids, negating the benefits of continuous ultrafiltration.
During MUF, ultrafiltration removes volume from the residual CPB circuit volume which increases its oncotic pressure. This high oncotic blood is then directed into the right atrium where it mixes with the patient’s blood prior to entering the pulmonary artery. This mixed blood enters the pulmonary artery with a slightly higher oncotic pressure than the rest of the body, pulling fluid from the pulmonary tissues where it is removed by the pulmonary capillary blood flow. This reduces pulmonary edema.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.