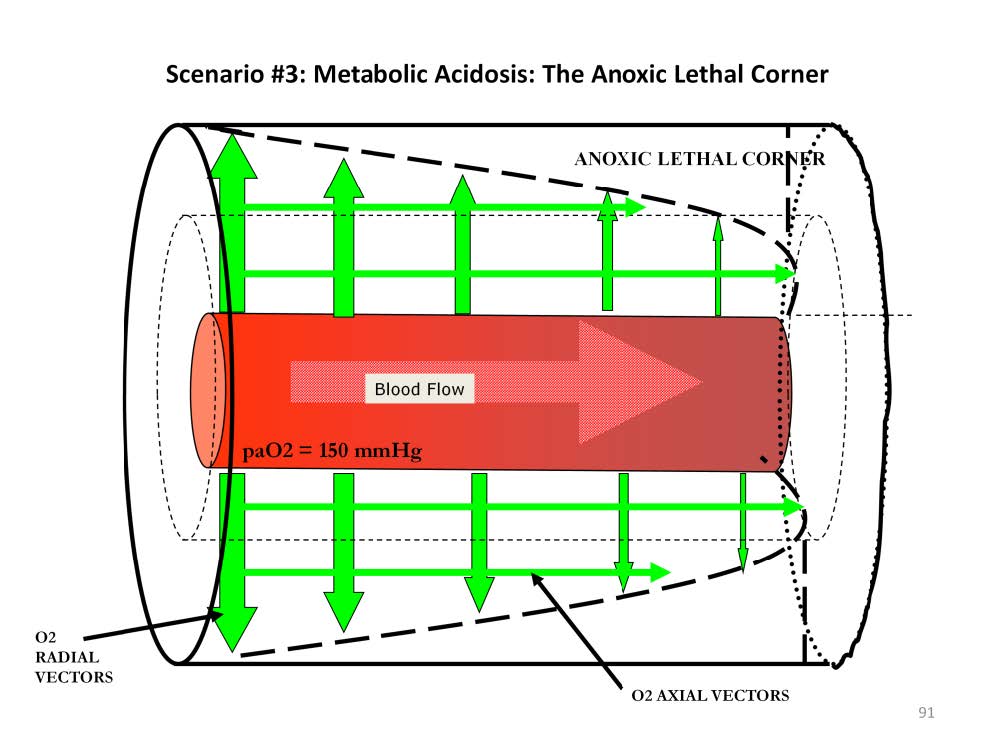
When intracapillary blood flow velocity is reduced below normal the result is a reduction in perfused capillary density and venous blood that has a lower than normal pvO2 concentration ( the SVO2 falls below normal). The oxygen concentration in the venous end of the Krogh cylinder falls below normal. However the arterial end tissues still receive adequate amounts of oxygen. This causes an increase in the axial gradient, pushing more oxygen towards the lethal corner area that has developed due to the de-saturated venous blood.
As intracapillary blood flow velocity falls, less oxygen comes from radial vectors and more comes from axial vectors. By the time that intra-capillary blood flow velocity reaches 25% of normal, 80% of the oxygen entering the venous end of the Krogh cylinder comes from axial vectors and only 20% comes from radial vectors. That’s not to say that there is adequate oxygenation at the venous end; only that most of the oxygen entering the venous end comes from axial vectors under these strenuous conditions.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.