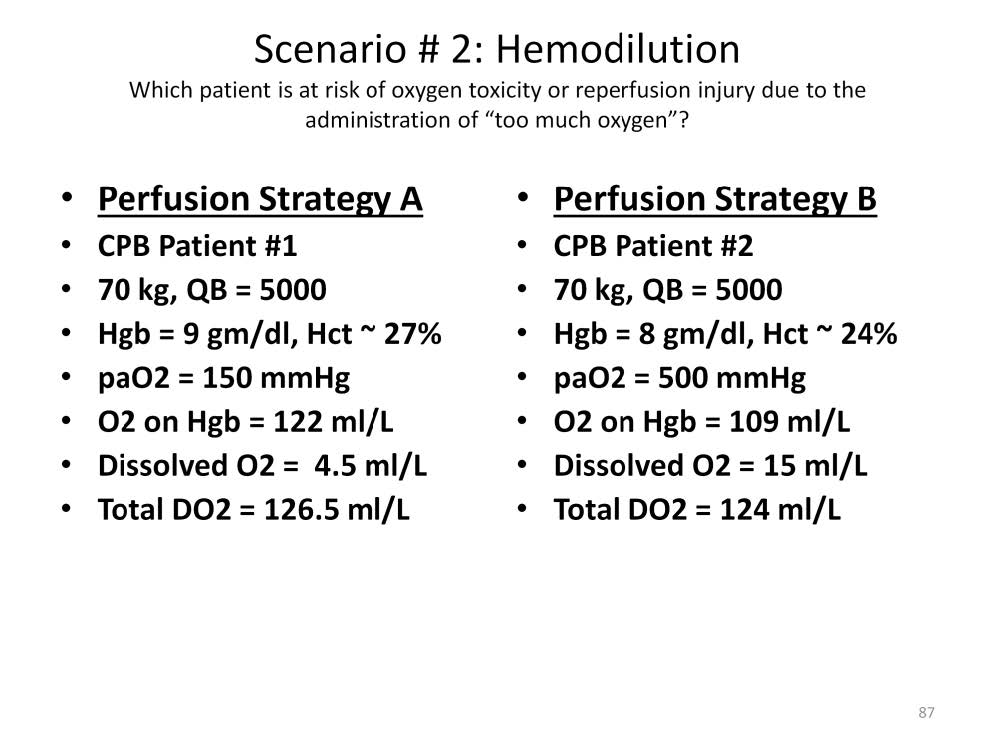
Two hypothetical patients with similar weights and calculated blood flow are treated with two different oxygenation strategies. Patient #1 has a hemoglobin of 9 gm/dl. To reduce the risk of oxygen toxicity or reperfusion injury, the paO2 is at only 150 mmHg. This gives a total oxygen delivery, including oxyhemoglobin and dissolved oxygen, of 126.5 mls/L of blood flow. Patient #2 has a hemoglobin of only 8 gm/dl. To improve oxygen delivery, the paO2 is at 500 mmHg. This gives a total oxygen delivery, including oxyhemoglobin and dissolved oxygen, of only 124 mls/L of blood flow. Even though patient #2 has a much higher paO2 than patient #1, the amount of oxygen delivered to patient #2 is less than patient #1.
If patient #1 were to develop a base deficit, the perfusionist may try to increase the oxygen delivery. The blood flow could be increased by 10% (to 5500 mls/min) or the paO2 could be increased to 500 mmHg. Either would increase the oxygen delivery by about 10%. If the blood flow cannot be increased due to circumstances and the paO2 is kept low due to fears of oxygen toxicity the perfusionist has three alternatives: 1) administer a buffer base which may simply mask the acidosis, 2) administer red cells to increase the oxygen delivery but which exposes the patient to transfusion hazards or 3) do nothing until the base deficit increases to an arbitrary limit beyond which intervention (items 1 or 2) must be taken.
By masking the acidosis with buffer base or ignoring it until it exceeds an arbitrary limit of acceptability, the perfusionist allows anoxic tissues to accumulate. At some point during or after cardiopulmonary bypass, these ischemic/hypoxic tissues will be re-oxygenated resulting in a genuine injury from reperfusion that the use of low paO2 values was initially trying to avoid.
The most common reason for acidosis on cardiopulmonary bypass is most likely the formation of an anoxic lethal corner due to a change in perfused capillary density. If blood flow cannot be increased, the best treatment is to address the lethal corner directly by using axial vectors to redistribute oxygen to the anoxic tissues. The administration of buffer base or red cells will not directly address the causative issue of the acidosis; the lethal corner.
If patient #2 were to develop a base deficit, the perfusionist may try to increase the oxygen delivery. The blood flow could be increased by 10% (to 5500 mls/min) but the paO2 is already maximized to 500 mmHg. If the blood flow cannot be increased due to circumstances, then the administration of red cells could be justified. The administration of red cells to patient #1 before applying the axial kick strategy may result in an unnecessary transfusion exposure.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.