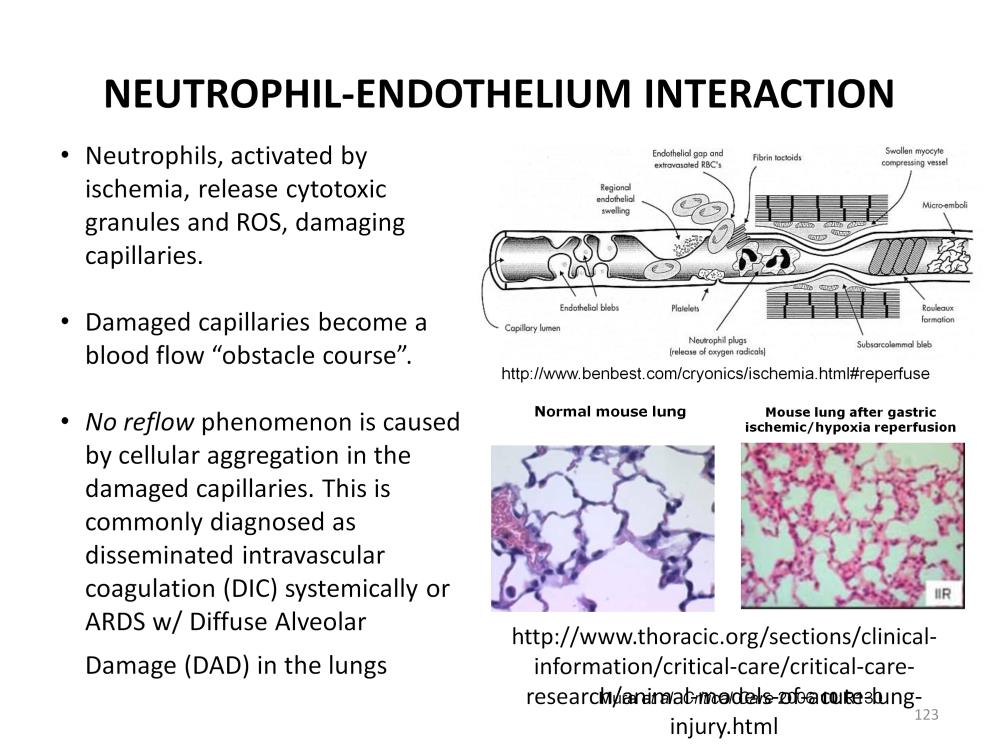
Neutrophils are activated during reperfusion, releasing cytotoxic granules and ROS. They can do significant damage to the capillary endothelium inside of the ischemic areas. In other non-ischemic areas such as the lungs, capillaries are subject to further attack by activated neutrophils. In an experiment by Mura et al, mice were subjected to gut ischemia by clamping of the gastric artery for 30 minutes after which reperfusion of the gut was allowed. Soon after gut reperfusion, the pulmonary capillaries became congested with activated neutrophils, damaging the lungs and severely compromising pulmonary function. This occurred even though the lungs themselves were not directly exposed to ischemia.
This is a form of ARDS which is the most common cause of death in the ICU, responsible for 50% of the mortalities. ARDS is usually associated with a ‘trigger’ such as trauma, burns, aspiration, blood transfusions, drug over dose, acute illness (cardiac arrest), pneumonia, sepsis, pancreatitis and many other conditions. However the common denominator associated with all of these things is shock. Patients in shock have under perfused capillaries and tissues which become hypoxic/ischemic. When these capillaries are suddenly reperfused during resuscitation, reperfusion injury is quickly manifested and often results in diffuse alveolar damage (DAD) and bilateral infiltrates in the lung (ARDS). The lesser form is called acute lung injury (ALI).
Besides damaging the capillaries, the neutrophils aggregate in vital areas, further damaging tissues and inhibiting normal perfusion. Capillaries damaged by reperfusion injury become an obstacle course to the smooth passage of red blood cells. Damage can include endothelial blebs, endothelial swelling, rupture, fibrin tactoids, activated platelets, swollen myocytes, subsarcolemmal blebs, rouleaux formation, and, of course, activated neutrophils. After the successful resuscitation and resolution of shock, this ‘no reflow’ phenomenon can result in a second round of localized ischemia and severely compromise perfusion of the organ systems. This is commonly diagnosed as disseminated intravascular coagulation (DIC) systemically and ARDS in the lungs. Externally this may appear as poor perfusion of the extremities with fingers and toes often turning purple and black from the blocked circulation.
Internally the effect can cause organ failure, and brain infarction and/or hemorrhage. Pulmonary hemorrhage after CPR followed by ECPR is a common complication. These hemorrhages are probably precipitated by activated neutrophils and subsequent no reflow phenomenon.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.