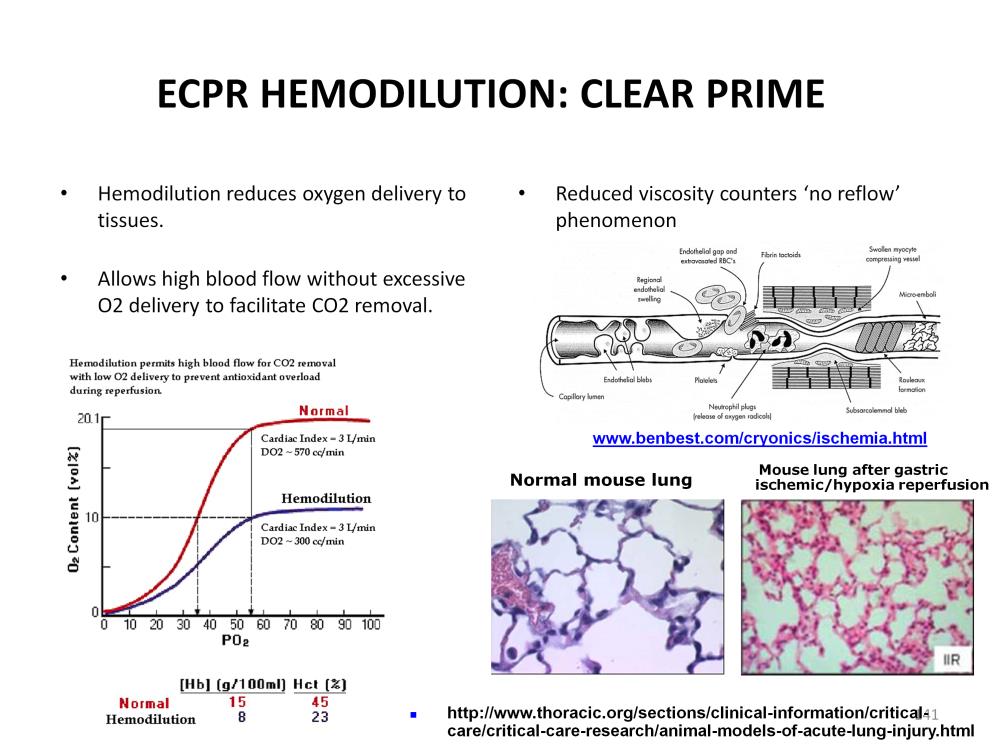
Hemodilution reduces the amount of oxygen that the blood can carry. This allows for a high pump blood flow rate without excessive oxygen delivery to the tissues where it can generate ROS in the RIP patient. High pump blood flow is needed to ensure quick core cooling and efficient CO2 removal from the tissues. However until these two protective strategies are fully implemented, the delivery of oxygen needs to be minimized. The chicken cardiac myocyte experiment demonstrated that continued anoxia is less lethal to ischemic cells than the sudden reintroduction of even moderate amounts of oxygen. Hemodilution is a method to prevent the reintroduction of excessive oxygen while allowing efficient cooling and CO2 removal.
Hemodilution also combats no reflow phenomenon. Blood with a low hematocrit is better able to navigate the obstacles present in damaged capillaries. Resuscitation CPR patients placed on extracorporeal support often manifest a pulmonary hemorrhage after a short period of time, from a few minutes to a few hours. This is probably due to a no reflow phenomenon in the lungs when blood is being pumped thru damaged capillaries that eventually rupture under the stress of perfusion. The same phenomenon can occur in the brain resulting in intracranial hemorrhage. Hemodilution may help to prevent this by reducing the high resistance to flow caused by thick blood traversing the damaged capillaries.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.