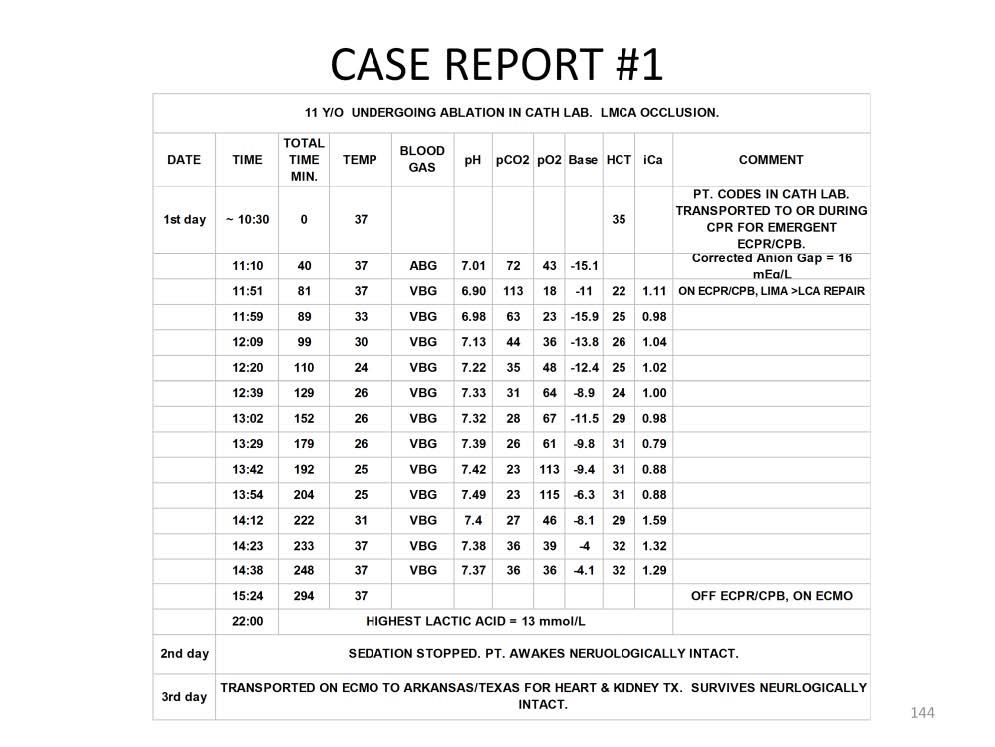
This is an illustration of how hypothermia, hemodilultion and hypocalcemia can be used to combat RIP. In this case report an 11 year old patient undergoing ablation in the cardiac catheterization laboratory experienced a sudden left main coronary artery (LMCA) occlusion necessitating the institution of resuscitation CPR. After 81 minutes of CPR the patient was placed on ECPR/CPB and immediately cooled to 24C while repairs were made to the LMCA. Venous blood gases drawn during this time period demonstrated the large amount of CO2 built up in the tissues during CPR, confirming the presence of RIP. This excess CO2 was removed as the patient was cooled, normalizing the venous pH and pvCO2 and reactivating intracellular antioxidants. Hemodilution was used to combat no reflow phenomenon, dropping the hematocrit from 35% to 22% after going on pump. The ionized calcium was kept low to reduce calcium stress.
While the patient was cool and after the venous pH and pvCO2 were normalized, the hematocrit was increased. Lastly during rewarming the ionized calcium was normalized. Cardiac function failed to return. Therefore the patient was transferred to a regular closed system ECMO pump for continued support. No pulmonary hemorrhage (a telltale sign of pulmonary reperfusion injury) developed. During the second day of ECMO support, the heart and kidneys were deemed irreversibly damaged. Sedation was stopped and the patient was allowed to awaken and found to be neurologically intact. The patient was subsequently transported on ECMO to a transplant center on the third day of extracorporeal support where she eventually received a successful heart and kidney transplant.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.