Polderman KH. Mechanisms of action, physiological effects, and complications of hypothermia. Crit Care Med 2009;37:S186-202.
“BACKGROUND: Mild to moderate hypothermia (32-35 degrees C) is the first treatment with proven efficacy for postischemic neurological injury. In recent years important insights have been gained into the mechanisms underlying hypothermia’s protective effects; in addition, physiological and pathophysiological changes associated with cooling have become better understood.
OBJECTIVE: To discuss hypothermia’s mechanisms of action, to review (patho)physiological changes associated with cooling, and to discuss potential side effects.
DESIGN: Review article.
INTERVENTIONS: None.
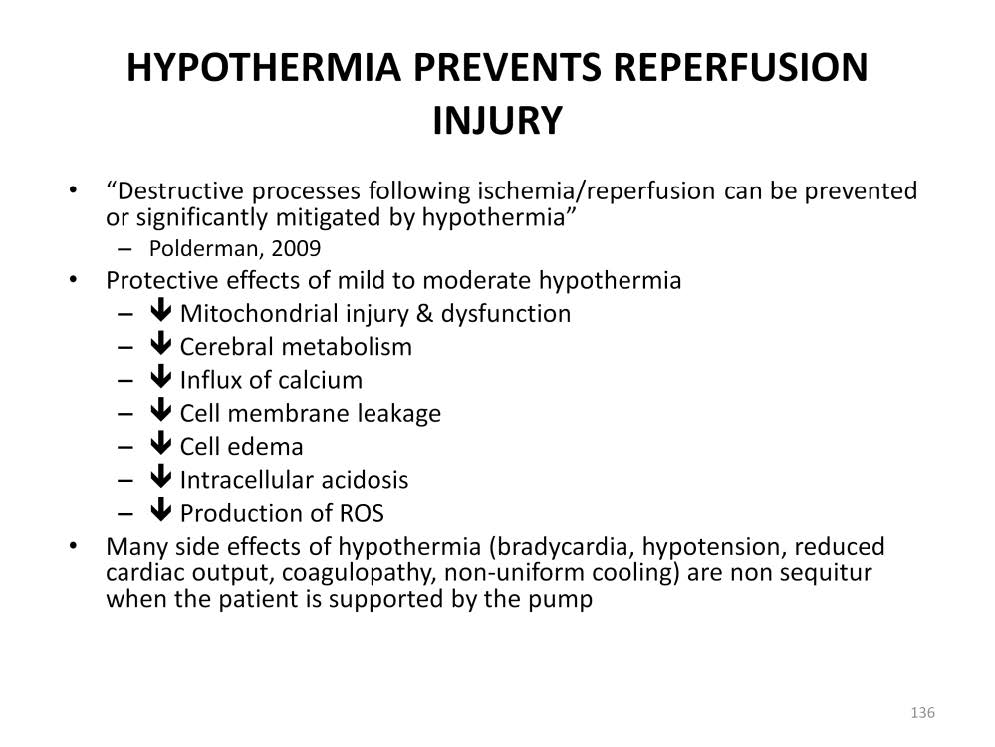
MAIN RESULTS: A myriad of destructive processes unfold in injured tissue following ischemia-reperfusion. These include excitotoxicty, neuroinflammation, apoptosis, free radical production, seizure activity, blood-brain barrier disruption, blood vessel leakage, cerebral thermopooling, and numerous others. The severity of this destructive cascade determines whether injured cells will survive or die. Hypothermia can inhibit or mitigate all of these mechanisms, while stimulating protective systems such as early gene activation. Hypothermia is also effective in mitigating intracranial hypertension and reducing brain edema. Side effects include immunosuppression with increased infection risk, cold diuresis and hypovolemia, electrolyte disorders, insulin resistance, impaired drug clearance, and mild coagulopathy. Targeted interventions are required to effectively manage these side effects. Hypothermia does not decrease myocardial contractility or induce hypotension if hypovolemia is corrected, and preliminary evidence suggests that it can be safely used in patients with cardiac shock. Cardiac output will decrease due to hypothermia-induced bradycardia, but given that metabolic rate also decreases the balance between supply and demand, is usually maintained or improved. In contrast to deep hypothermia (<or=30 degrees C), moderate hypothermia does not induce arrhythmias; indeed, the evidence suggests that arrhythmias can be prevented and/or more easily treated under hypothermic conditions.
CONCLUSIONS: Therapeutic hypothermia is a highly promising treatment, but the potential side effects need to be properly managed particularly if prolonged treatment periods are required. Understanding the underlying mechanisms, awareness of physiological changes associated with cooling, and prevention of potential side effects are all key factors for its effective clinical usage.”

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.