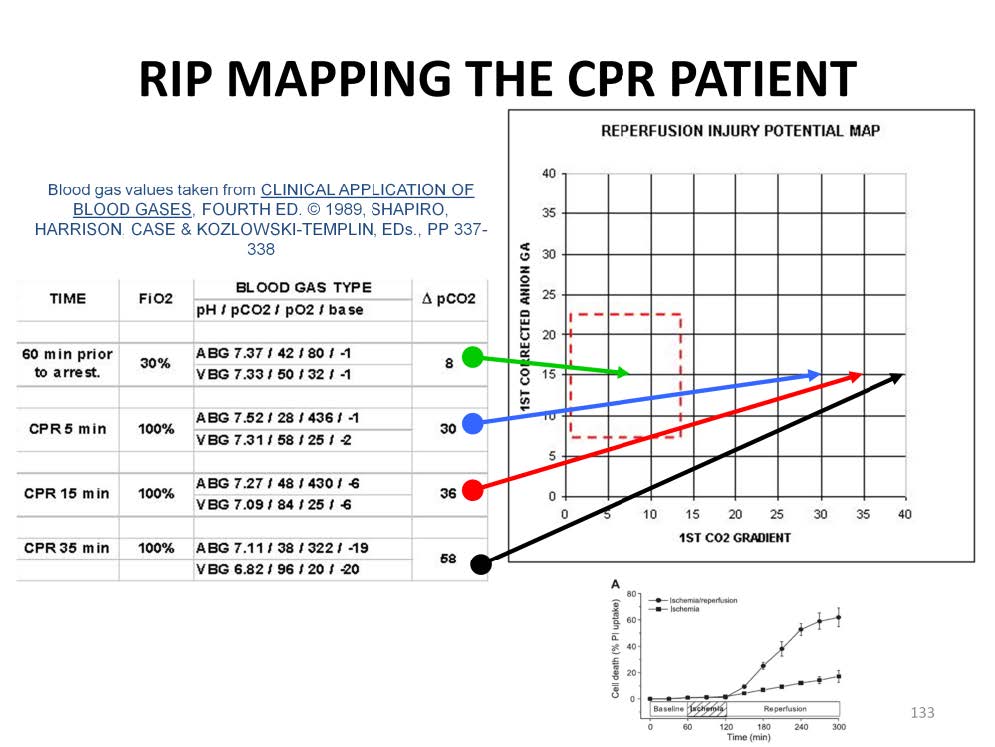
Typically patients undergoing resuscitation CPR will experience a great increase in their venoarterial CO2 gradient. This is caused by a slowing of the blood flow thru the capillaries and the resultant ‘backing up’ of CO2 in the tissues. In order to make this measurement, an ABG and a central VBG need to be drawn at the same time. The real-life example illustrated above shows the typical pattern seen in a patient undergoing resuscitation CPR for 35 minutes.
The first set of blood gases prior to arrest shows the patient with normal oxygen and CO2 levels, normal pH and base balance. The venoarterial CO2 gradient of 8 mmHg, located in the midpoint of the lane, correlates to a tissue pCO2 of 74 mmHg. Formula paCO2 + (4 X p[v-a]CO2): 42 + (4 X 8) = 74 mmHg tissue pCO2.
Five minutes after resuscitation CPR is started, the CO2 gradient climbs to 30 mmHg (almost 4 times normal). This plots well outside of the lane and demonstrates that even early in the resuscitation period the patient is developing RIP. Under poor perfusion conditions such as this, the tissue pCO2 increases more than the gradient increase. In other words, a rise in the gradient from 8 to 30 mmHg (a 22mmHg increase) causes a rise in the tissue pCO2 from 74 mmHg to 148 mmHg (a 74 mmHg increase). Notice how the paCO2 appears hypocapnic while the pvCO2 is hypercapnic.
After 15 minutes of CPR, the CO2 gradient is 38 mmHg, relating to a tissue pCO2 of about 192 mmHg.
After 35 minutes of CPR, the CO2 gradient is 58 mmHg relating to a tissue pCO2 of about 270 mmHg.
The large increases in tissue CO2 correlate with intracellular acidosis which is a precondition for RIP. It is not necessary to actually make these ABG & VBG measurements to determine if RIP is developing in a resuscitation CPR patient. The increase in the venoarterial CO2 gradient is an inevitable consequence of CPR, so that after 10-15 minutes all patients will be out of the lane and subject to RIP. If the decision is made to place a patient like this on an ECMO pump, a reperfusion strategy should be used to prevent the lethal reperfusion injury that will occur upon the initiation of extracorporeal support. In addition, since the accumulation of tissue CO2 can be quite large, the risk of reperfusion injury will last until the CO2 gradient can be brought within the lane. This could take many hours.
As previously described the sudden reintroduction of oxygen into anoxic cells can be more deadly than allowing the anoxia to continue while a strategy is formulated to prevent the reperfusion injury form occurring. While not plotted on this example, the anion gap (and even the lactate) may or may not remain within acceptable limits during this relatively short resuscitation time frame.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.