As explained earlier, the institution of normal hematocrit, normal temperature ECMO in a patient with RIP can greatly increase the risk of death. Without a VI score, it is difficult to determine which patients have RIP and to what degree, since all of these patients need extracorporeal support. If it is determined that a patient has RIP, some strategy besides traditional ECMO needs to be employed to address the ramifications of RIP.
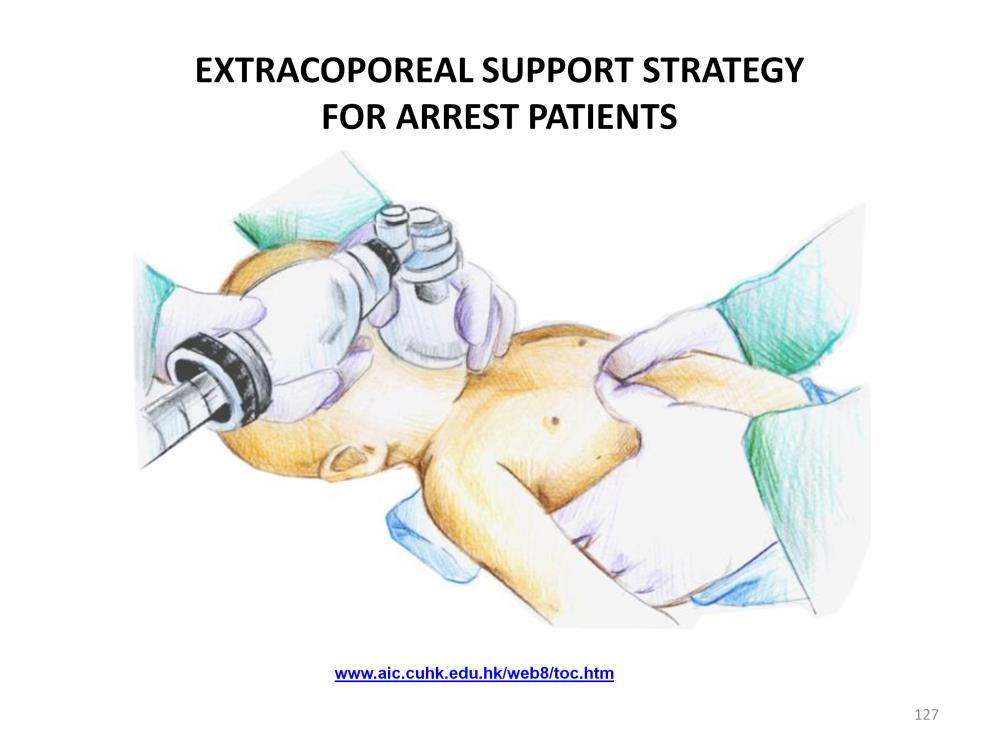
One type of patient who most certainly has RIP is the coding or near code patient. This patient is almost always outside the lane before ECMO can be initiated because RIP develops within a very few minutes due to poor perfusion from CPR. A strategy called ECPR (extracorporeal cardiopulmonary resuscitation) can be utilized in these patients to address each of the four reperfusion injury mechanisms.
The terminology for this type of extracorporeal support is by no means standardized. It has also been called emergent ECMO (E-ECMO), rapid deployment ECMO (RD-ECMO) and extracorporeal (or emergent) cardiopulmonary support (ECPS). These terms merely denote the rapid implementation of a pump-oxygenator to support a dying patient. However for this presentation, ECMO will mean the initiation of traditional normal hematocrit, normal temperature extracorporeal support and ECPR will mean the initiation of a strategy of extracorporeal support using hypothermic hemodilution and hypocalcemia to prevent reperfusion injury.
The typical resuscitation of a patient in severe shock or who has already had a cardiac arrest centers on the goal directed therapy of normalizing cardiac output, blood pressure, arterial oxygen saturation, arterial blood pH, etc. However attempting to resuscitate a patient in this manner without an understanding of the ramifications of reperfusion injury is like treating an infection without knowing anything about bacteria. The results will be ‘hit and miss’.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.