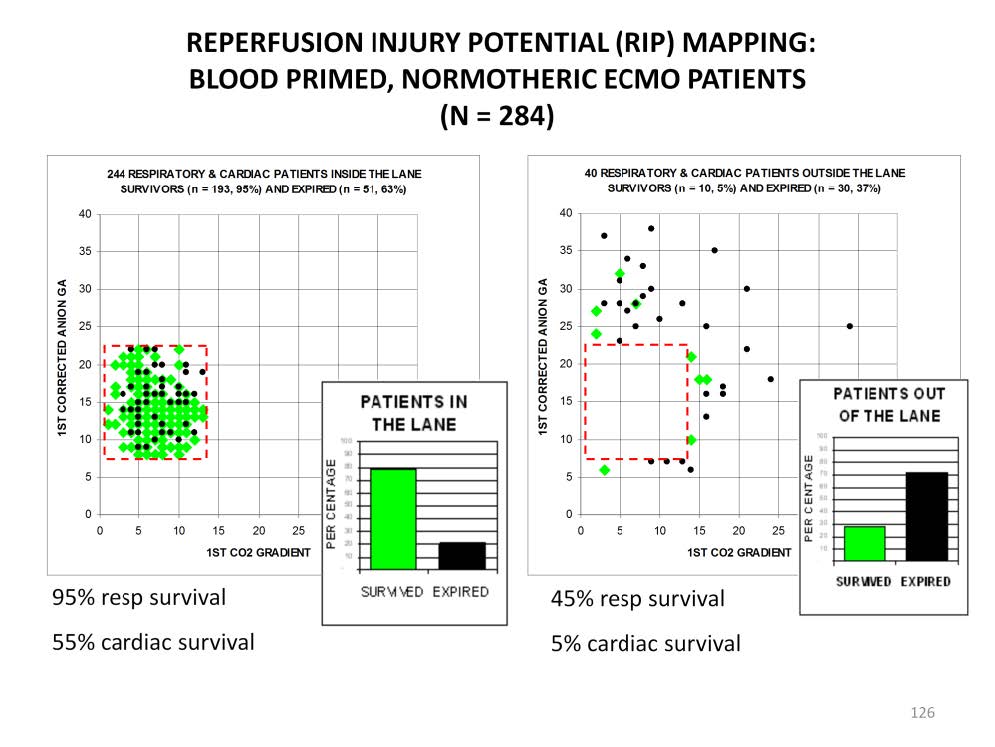
The level of shock that a patient is enduring can be determined using the Viability Index (VI). The VI is calculated by adding the corrected anion gap and the venoarterial CO2 gradient together. The high VI scores correlate to a high the level of shock. This, in turn, relates to a high level of RIP. The VI can be charted on a grid (see the charts above). These charts contain the first VI score just after patients were placed on traditional, blood primed, normothermic ECMO.
The patient population was pediatric with most patients weighing less than 10 kg. The diagnoses varied in 2 broad categories; respiratory and cardiac. The respiratory diagnoses included all the traditional neonatal ECMO conditions (with the exception of congenital diaphragmatic hernia); meconium aspiration, primary pulmonary hypertension, respiratory distress syndrome and sepsis. In older patients, diagnoses included primarily pneumonia, respiratory syncytial virus, sepsis and trauma. The most common cardiac diagnoses included pre and post surgery for congenital heart disease and cardiomyopathy.
The VI scores of 95% of the survivors fall into a relatively small area between the corrected anion gaps of 7 and 22 mEq/L and the venoarterial CO2 gradients of 1 and 13 mmHg. This small area is known as the “lane” in reference to the rectangular area beneath a basketball goal from which a player is most likely to make a goal. In contrast, only 61% of the expired patients’ VI scores are located in the lane. The overall mortality for patients in the lane is 21%.
Only 5% of the survivors are located outside the lane along with 39% of the expired patients. The patients outside the lane have a mortality rate of 73%. This mortality rate is 3.5 times higher than for patients in the lane. Why such a difference? The VI scores indicate that the patients outside the lane are at a higher level of shock than patients in the lane, therefore they have more RIP. When these patients are placed on ECMO using a blood prime (normal hematocrit levels) and normothermia, the sudden reperfusion of previously ischemic tissues results in reperfusion injury. This can manifest itself in many ways; brain hemorrhage or infarction, pulmonary hemorrhage, cardiac stun, renal failure, multiple organ failure or, simply failure to improve or heal from the original underlying pathology.
Not all patients needing ECMO support have RIP. Indeed hypoxic neonates tend to be resistant to RIP which is probably why neonatal ECMO has been so successful. However older patients with non-neonatal diagnoses are less resistant to RIP and have much poorer survival when placed on ECMO. In many of these patients the use of ECMO has the potential to cause a lethal reperfusion injury which ,in addition to the risk of the underlying disease, adds greatly to the risk of death.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.