Swenko by Gary Grist RN CCP Emeritus with Kelly Hedlund MS CCP and the AmSECT History Committee
Gastric Freezing
Successful repair of congenital heart lesions in the early 1950s performed by Drs John Lewis and Walton Lillehei using hypothermic inflow occlusion and cross circulation was only possible with support from their surgical chief, Dr. Owen Wangensteen (1). This same Dr. Wangensteen of the University of Minnesota Medical Center developed a method to treat gastric ulcers with topical hypothermia, which was, in essence, gastric freezing (2). A local refrigeration appliance manufacturer, the Swenko company in Minneapolis, constructed a cooling device to recirculate subzero alcohol through dual tubes connected to an inflatable, stomach-shaped balloon. The deflated balloon and tubes could be introduced through the mouth and esophagus into the patient’s stomach. Once there, the Swenko machine would recirculate the freezing alcohol to inflate the balloon and bring it into contact with the gastric ulcer to freeze it therapeutically. Extreme hypothermia was thought to cure the ulcer by disabling the acid-secreting cells in the stomach. Figure 1 denotes “water,” but the actual cooling medium used was ethyl alcohol to achieve subzero temperatures.
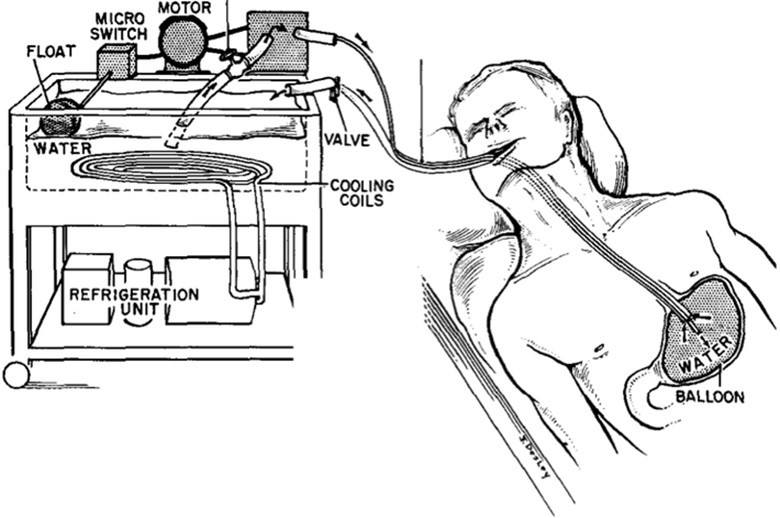
Figure 1 Swenko gastric freezing device in use. Schematic drawing of the device employed for obtaining local gastric hypothermia. In Wangensteen O, Root H, Jenson CB, et al. “Depression of Gastric Secretion and Digestion by Gastric Hypothermia: Its Clinical Use in Massive Hematemesis.” Surgery 44, no. 2 (1958): 265-74, illus. p. 270.
Swenko Is Born
Thus, the Swenko Research and Development Co. was born. Swenko is a combination of the owners’ names. Emil Swenson and William Koski were both commercial refrigeration service engineers. In 1957 Swenson and Koski opened a store in Minneapolis to sell and service home appliances. By 1962 they were developing the gastric freezing device with Dr. Wangensteen. Soon thereafter, Swenko worked with Dr. John Feemster, also of the University of Minnesota Medical Center, to create an organ preservation machine based on the use of hypothermia and hyperbaric oxygenation for preservation (3). It was thought that hypothermia along with hyperbaric oxygenation would extend the safe storage time for organs for 24-72 hours.
Figure 2 Swenko organ preservation machine with three hyperbaric chambers for multiple organ storage.
On The Kidney Transplant Team
Early in my career as a perfusionist, in 1968, I was a part of my hospital’s kidney transplant team. A perfusionist was on the kidney transplant team to operate the Swenko, an organ preservation machine. This was at the dawn of organ transplantation in the USA. Only kidney transplants were being performed at my hospital, no hearts, lungs, or livers. There was no United Network for Organ Sharing (UNOS), a private, non-profit organization that universally manages the U.S. organ transplantation system from procurement to transplantation. Back then, my hospital was acting independently and learning as it went. As part of our daily routine, transplant team members would scan the newspapers for reports of automobile accidents and, in particular, motorcycle accidents whose victims might have severe brain damage. (This was before any helmet laws.) We called various hospitals to obtain information on accident victims who might be potential kidney donors. Back then, ICU nurses would freely give family, friends, and other healthcare workers information on a patient’s condition. We were looking for brain-dead donors whose families could be approached about organ donation.
My Swenko
An integral part of my particular Swenko machine was a single stainless-steel, blunt-bullet-shaped hyperbaric chamber of about 1 gallon in volume with a heavy-duty screw-on lid that could withstand pressures of 2-3 atmospheres of pure oxygen. The chamber fit into the top of a stainless-steel chest filled with ice to cool to 2-4 degrees centigrade. The kidneys would be placed in the chamber with IV tubing secured to the renal arteries. This tubing was secured to the underside of the lid with a special fitting. Then more IV tubing was connected from the chamber top, which allowed the preservation solution to be slowly dripped into the kidneys. As the chamber was first flushed with oxygen and then pressurized to 30-60 psi, a special IV pump would push the preservation solution into the kidneys under pressure. An oxygen E tank was affixed to the side of the chest and there were handles on the side that allowed the entire contraption to be lifted and carried. The assembled unit was quite heavy with the chamber, chest, ice, IV solutions, IV pump, and oxygen tank.
“Late To The Party”
For after-hours donors, while others on the transplant team (surgeons and nurses) proceeded directly to the donor hospital from wherever they happened to be, the perfusionist was required to pick up the equipment from the home hospital before proceeding to the donor hospital. The perfusionist on call was notified by beeper (there were no cell phones back then) to gather the Swenko equipment (which also included the instrument pack that the procuring surgeon would use) at the home hospital and then go to where the donor was located. The team sometimes joked that I was “late to the party” because there were a few times when the donor’s heart stopped before I could get there, and the surgeon elected not to procure the kidneys due to the ischemic time involved.
No Organ Bank
Since there was no organ bank and mine was the only hospital doing kidney transplants in the city, it had to do the tissue typing as well. Recipients with donor-compatible blood types were called and told to remain NPO (nothing by mouth). When the kidneys were collected, blood specimens were also collected for tissue typing upon return to the home hospital. When this was completed, the best recipient was called into the hospital for transplantation. Often, we had two kidneys, so two recipients were called, and two transplants were performed. Once back at the home hospital, the task of slowly decompressing the kidneys within the Swenko was timed to be completed just as the surgeon was ready to implant the organ.
Swenko Abandoned
I always felt uncomfortable about decompressing the kidneys and worried about gas emboli forming in the organs and damaging them. Eventually, we figured out that our kidneys were always transplanted within 8 hours, so extended storage time was not needed. Subsequently, hyperbaric oxygenation along with the heavy Swenko was abandoned on our part. But it was not until the mid-1970s that hyperbaric oxygenation for organ preservation was generally abandoned (4).
Richard Jensen
Richard Jensen, the first president of AmSECT, presented a History of Perfusion lecture at the 41st International Conference in Las Vegas in March 2003. Below is a humorous excerpt from that talk concerning gastric freezing. (JECT. 2003;35:270–273)
“We did our payback to Dr. Wangensteen and his gastric freezing for bleeding ulcers. The cooler was a Sweden Freeze ice cream machine we adapted to almost freeze alcohol through tubing and a pouch shaped like a human stomach. Two brothers from Indiana had eaten too much spicy chili and beer. After their surgeries, they went home happy and were told not to drink beer or eat spicy chili. Later, on the front page of the Chicago newspaper, there was a color photograph of the two of them with their chins over a big pot of chili. (So much for following their doctor’s orders!) We also had a priest come in for the freezing, then he started singing and we had to ask the Mother Superior to leave because his singing became very bawdy. When I started warming and deflating the balloon, we found a pinhole in the balloon; which explains why the priest was a very happy patient.” (….from the alcohol leak, no doubt! G.G.)
Swenko Only Placebo
In the 1980s, the bacterium Helicobacter pylori was shown to be the cause of peptic ulcers that needed to be treated with antibiotics rather than surgery. But even before that, in 1965, the benefits of gastric freezing were proven to be only a placebo effect, and the practice was soon abandoned (5,6). By 1984 Swenko was out of business as a medical machine developer.
