Part XXVII – Random Thoughts – Standing on Tall Shoulders – The History of Cardiac Surgery – Thomas N Muziani PA-C, CP
“The two most important days in your life are the day you were born and the day you find out why”- Mark Twain
A Thought Experiment:
In attempting to re-focus on the history of cardiac surgery I discovered a collection of disparate information impossible to compartmentalize. My sole intent, at the very least, is to provide contemplation and hopefully discussion.
Disparate Info #1: Whole Body Wellness;
Dr. Pamala Taub MD, FACC, is the founder and director of Step Family Foundation Cardiovascular and Wellness Center at University California San Diego’s Jacobs Medical Center. This Wellness Center is the first of its kind at a major medical center with an intense focus on whole-body wellness, which includes diet, exercise and preventative care.
While her clinical practice concentrates on preventive cardiology and lipidology, her research; which has received funding from the National Institutes of Health, the Department of Defense and the American Heart Association; focuses on assessing how pharmacologic intervention along with lifestyle changes may affect cardiometabolic disease.
Since 2018, Dr. Taub has been working with Dr. Satchidananda Panda, a professor at Salk Institute’s Regulatory Biology Laboratory in La Jolla, California, to study the effectiveness of circadian-rhythm-based diet intervention on cardiovascular health, compared with conventional behavior counseling.
Here are the thought-provoking, pragmatic observations;
For almost all of human history, our species has depended upon the limited hours of daylight available to hunt, scavenge or roam for food. Therefore, almost every cell in our body still maintains a biological clock that tells us when to be active- utilizing the nutrients from food to grow and conduct normal business…and when to rest. There is now growing evidence that validates disruptions to this natural cycle, triggered by artificial light and round-the-clock access to food, directly impacts our health, resulting in everything from poor quality sleep to obesity, heart disease, diabetes and cancer.
Within the span of this author’s lifetime, there has been a major transformation in the overall physiologic profile of the average cardiac patient. During the 1950’s and 60’s, smoking, especially non-filtered cigarettes… “they just taste better” touted the commercial jingle, was extremely popular and very chic with both men and women. Smoking indoors around little children or babies was a non-issue. It was also very chic to imbibe hard liquor, without consequence, during any hour of the day or night. Fatty beef and starch heavy meals were perceived as a sign of affluence.
The outcome was a population that either died prematurely or led a rather healthy lifestyle into old age. Most patients that presented for cardiac surgery were younger than 70 years old, diabetics were rare (childhood diabetes was non-existent) and re-dos were seldom. But it was not atypical to open a chest and discover global carcinoma on both lungs, or a forty-five-year-old individual whose body looked like a pathological museum piece thoroughly pickled and ready for display at Madame Tussauds.
Nature and Darwin have proven throughout our evolution; adapt or die. We may fully comprehend the ramifications of excessive smoking, but it is rather a simple mind trick to modify that oral fixation to accommodate something less odious…like food bingeing.
Today, the average refrigerator in the United States is easily accessible and way too large…we feel an almost sub-conscientious need to keep it full. Pre-processed foods and soft drinks are intentionally developed to be too convenient, too sugary, too salty and too tasty. This is repeating the exact same dogma that cigarette manufacturers admitted to during Senate Hearings in the 1960’s on how they formulated the acute addiction to cigarettes. Their concern was never about the health and welfare of the consumer. It was all about selling more cigarettes. Quote of the 1980’s; “Greed is good.”
Clustered co-morbidities, prior interventions and an aging population are now the standard patient profile. Then, in the proverbial axiom: “adding insult to injury”, many cardiologists will only allow a patient to have his/her “chest cracked” (the phraseology used by a cardiologist to dissuade his patient from going to a surgeon) when A) the patient is ready for a priest’s entrance stage right, B) Cardiology cannot afford another negative outcome or C) It’s Friday, a Holiday or the Cardiologist has a dinner date. Then, he will hand the patient off to surgery. As Isaac Asimov once wrote: “Life is pleasant. Death is peaceful. It’s the transition that’s troublesome.”
Disparate Info #2: STS Database for 2018:
In the never-ending quest at improving outcomes, this information from collected data at the Society of Thoracic Surgeons might be of some use. For individuals outside of the United States, this information may assist in targeting specific areas for addressing improvement.
In Hospital Mortality in the United States:
Expressed as overall averages:
- Within normal limits arresting times. The STS statistics presented reflect “normal” x-clamp times (1-3 hours). Longer x-clamp times skew mortality figures dramatically. Number one increase in mortality is extended (3-5 hours) x-clamp without complete protection. This is why people who use del Nido have to be very careful about keeping the heart cold throughout the entire x-clamp period.
- 1 to 3% for CABG
- 6% Adult Valve Surgery
- 5% Pediatric Surgery
Morbidity:
- Ventricular Arrythmia’s Common
- Coronary Vasoconstriction (spasm)
- Left Ventricular Stunning- 10%
- Post-op Atrial Fibrillation- 25-40%
- Renal Dysfunction- 10-40%
- Neurological Damage- 10-40%
- Longer Hospital Stays- 10-40%
- Inflammatory/ Coagulation Imbalances
- Increased Healthcare Costs associated with extended stays
Disparate Info #3: Ventricular Fibrillation and High Sensitive Troponin T:
A rather large study (10,000+ patients) conducted at six hospitals in Germany, one in Croatia and one in Italy on the release of High Sensitive Troponin T (proteins in the troponin complex integral to contraction in cardiac myocytes) during cardioversion concluded an interesting finding; the causation for the release is not due to physiological changes generated by ventricular fibrillation as was universally believed. They isolated the trigger point to the act of electrically shocking the heart with implantable defibrillators.
This author has written numerous times regarding the concerns with applying metallic conducting paddles directly upon a human bare heart plus acting cavalier regarding the number of joules released. I believe all of us by now are well acquainted with the end effect of electrical shock therapy administered directly upon the human brain. Same medieval concept…different organ. Now transfer that same mindset to a highly sensitive organ that is totally dependent upon very delicate electrical information to trigger a syncopated rhythm.
The last thirty-five years have provided empirical validation at numerous institutions that applying defibrillator patches and attaching the appropriate cable to your patient prior to surgery should be standard operating procedure. Skin is a wonderful safe conductor and the distance from the heart appears to attenuate any gross electrical ramifications imposed upon the myocardium.
In the event of an arrest, either with the chest open or closed, all the circulating nurse, anesthesia or perfusion has to do is charge the paddles and push the button. Oh! And please yell: “CLEAR!” No more “Grey’s Anatomy” theatrics and no surgeon taking his frustrations out with adjusting too high of joules. We had a rather well-known Argentinian surgeon who would scream during a cardiac arrest: “Hurry! Hurry! The patient’s going to Die!” Just imagine a poor patient in the next room, about to go to sleep and hearing that proclamation. Plus, at our institution, ICU nurses truly appreciated having the patches already applied prior to the patient’s arrival. It makes for a seamless transition from operating room to intensive care.
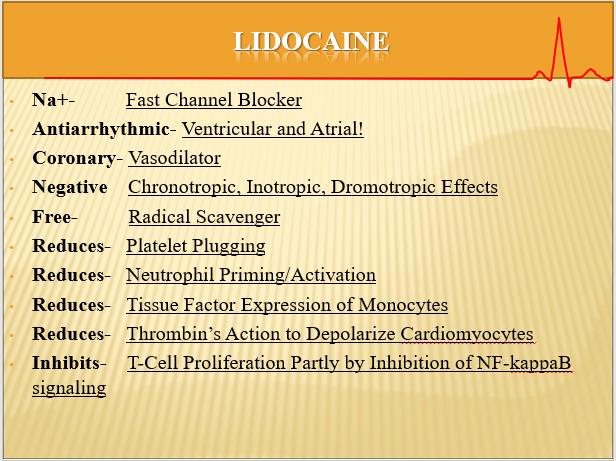
Disparate Info #4: The Benefits of Lidocaine and Magnesium in Cardioplegia:
As with my all-time favorite axiom: “All bleeding stops…eventually” …words of advice about cardioplegia ingredients. If you are contemplating adjusting or re-thinking your cardioplegia formula, please spend a little time investigating incorporating Lidocaine and magnesium into your solution matrix. Please do not inject drugs directly into the cardioplegia bag. Doing so may void any warranty on sterility and/or stability. Contrary to popular belief, an oxygenator does not perform like a Cuisinart…it has no mixing setting. Always inject Lidocaine slowly (i.e. 1/3, 1/3, 1/3) to avoid arresting or 1st degree block.
These two drugs have proven over the last forty years to provide remarkable myocardial protection throughout the entire quiescent cycle. As a side note; Procaine is not a substitute for Lidocaine. Hyperkalemia will not shut down membrane-ion pumps during quiescence. Lidocaine will. Please remember that magnesium works synergistically with Lidocaine in creating reproducible positive protection during all phases of myocardial protection no matter what temperature the myocardium. Included are three slides on the subject in an effort to illustrate.
See references below.
See references below.

See references below.

Interesting article even for a non-medical person. Thank you.
Mr. Hurzeler,
Your opinion means more to me than you will ever know. My hope has always been to have the thoughts expressed discussed by everyone. Thank-you for your input. T
Timely article as we are discussing changing our cardioplegia solution. Some of the points you mentioned have been part of our discussion and I will use your article to support some of my concerns.