A Face Full of Blood by Gary Grist RN CCP Emeritus
Pet Peeve
I will use this article to address a pet peeve that I have had for over 50 years; the lack of eyewash stations at scrub sinks in ORs. How many of you have seen eyewash stations in the OR? I have worked in four different hospitals and visited many more. But I have never seen eyewash stations at the scrub sinks or anywhere in OR clean areas where perfusionists work. I have stewed about this for decades. If you have eyewash stations, you are lucky!
Bloody Career Splash
Many perfusionists will get grossly splashed in the face with blood projected under pressure at some point in their career. I did it to myself when I was careless. Or it can happen at the hands of a co-worker who also was careless. It can occur during an emergency, like changing an oxygenator or repairing a circuit disruption. I think it most frequently occurs when dismantling a pump after use. There is no national registry to report such incidents, so I am not sure of the frequency of this type of gross blood contamination. But I guess that a perfusionist averaging 200 cases/yr will have a gross blood confrontation about every five years.
Ron Stetzer Cartoon
Most perfusionists have seen the cartoon “OOPS!” showing two perfusionists working at a pump that is exploding and showering them with blood. The cartoon was by a commercial artist named Ron Stetzer. It was featured in the first issue of The Journal of the American Society of Extracorporeal Circulation Technicians in early 1967. For a brief time, Ron worked at the University of Pittsburgh in the Medical Illustration Department, designing charts and graphs for presentation and publication. He no doubt had a connection with somebody who worked with exploding perfusion circuits. Such an incident may have seemed comical at the time. But the expressions on the perfusionists’ faces bring to light the unexpected and unanticipated nature of the pressurized blood spill. And the risk of contracting a serious blood-borne infection is no laughing matter. The pump depicted in the cartoon is a caricature of the kind I first used in 1968. The risk of blood spurting from a circuit into a perfusionist’s face is still an ever-present possibility over 50 years later.
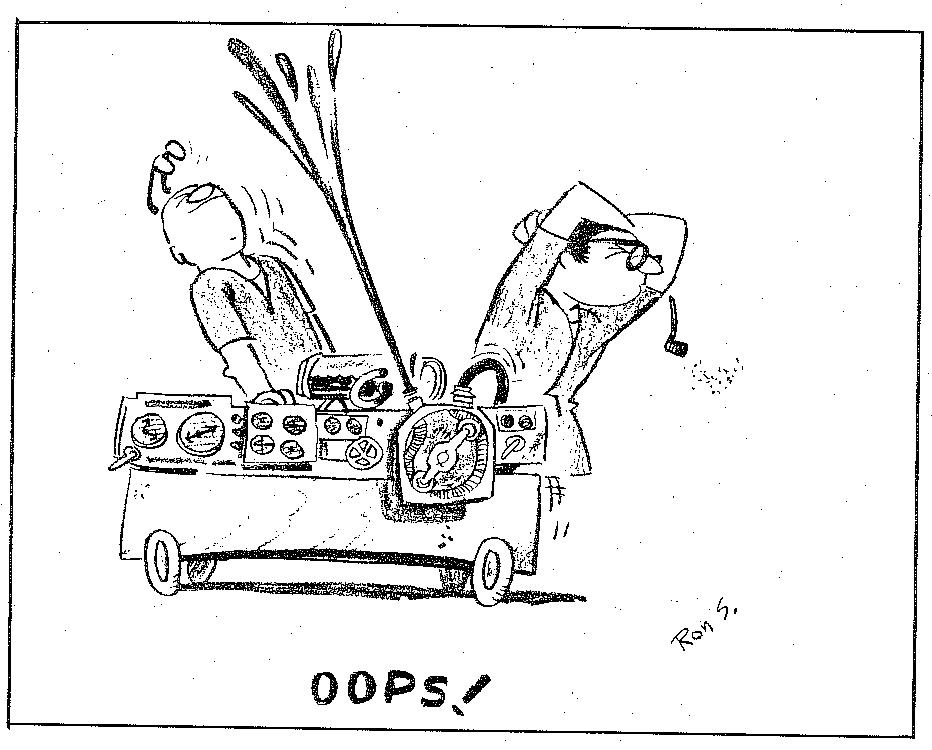
Ron Stetzer “OOPS!” Perfusion Cartoon
Personal Protective Equipment (PPE)
PPE is required in all ORs. But the thin paper masks, some with attached flimsy eye shields, and other types of eyewear provided are only designed to protect against bloody aerosol or droplet contamination. They won’t protect against a blood spill under pressure like that shown in the cartoon. Full face shields are a little better, but I did not like wearing them during the case because they impair communication with others. The wrap-around shield diverts sound away from your ears, and, worse yet, it blocks the volume and clarity of your own voice more than the usual paper mask. Failure to communicate clearly is probably the number one cause of errors in the OR. Face shields should be worn when contamination to the face is most likely, and communication is not an important factor: during circuit tear down.
No Support Or Requirement
When I talked to surgeons about getting eyewash stations installed at scrub sinks, their attitude was something like this; “If you choose to work in surgery, you should expect to get blood in your eyes and face on occasion. So, live with it!” This seemed like a malediction to me since we have all seen surgeons get a face full of blood when cannulation goes wrong. When I asked hospital administrators, architects, and engineers about installing eyewash stations, they said that there was no specific Joint Commission (JC), Occupational Health and Safety Administration (OSHA), Centers for Medicare and Medicaid Services (CMMS), or Association Of Operating Room Nurses (AORN) requirement for eyewash stations in the OR for blood contamination; the lab yes, the OR no. So, without surgeon support, I could not get OR eyewash stations at my old hospital. Even when specialty rooms for ECMO were built in the ICU, I tried to get eyewash stations installed there. No go, despite the occurrence of several ECMO ICU nurses getting splashed in the eyes despite their PPE during the three decades that I was active in our ECMO program.
What Does OSHA Say?
I could write a lot about OSHA requirements* to protect workers from blood-borne pathogens. You can look them up for yourselves online. But I am trying to keep this as short and straightforward as possible and focused on eye and face contamination. I think it is sufficient to say that OSHA, JC, CMMS, and AORN, for that matter, do not specifically mention the requirement for eyewash stations in operating rooms. Not even in the AmSECT Standards and Guidelines is there any mention of a perfusionist’s safety from a pressurized blood spill to the face. Add to that the risks from ever more caustic sterilizing solutions and the increased frequency of decontamination procedures required for heater/coolers. The need is clearly there. It’s just that nobody seems to want to do anything about it. And it is not just perfusionists at risk. I would guess that in any large, multi-room OR, someone (a surgeon, anesthesiologist, nurse, scrub tech, or cleaning crew member) gets blood in their eye, nose, or mouth every week. You’ve all seen someone trying to rinse the blood away from their face under a scrub sink faucet. You probably have done that yourself. *OSHA’s Bloodborne Pathogens standard (29 CFR 1910.1030)
https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.1030
When Are Eyewash Stations Required?
OSHA requires eyewash stations wherever there is a possibility that caustic or corrosive chemicals could splash into the eyes. And eyewash safety stations must be installed within 10 seconds or 55 feet from the hazard. So, technically, heater/cooler decontamination should be performed in some place where there is an eyewash station. But blood and body fluids are not considered to be caustic or corrosive by any authoritative entity. And I do not think the use of PPE negates the need for an eyewash station, and OSHA agrees with that contention. But accreditation organizations like JC and CMMS do not require or specify the location of eyewash stations in cases of blood contamination. The facility, at its option, is expected to conduct a risk assessment to determine if and where eyewash stations are needed. Perfusionists should take the lead in conducting such a risk assessment and bring it to the attention of the proper in-house authority. But, if a facility does not conduct such a risk assessment, they are not in violation of any JC or CMMS regulation. And yet, in most applicable policies and procedures for exposure to blood-borne infections, it usually states that the victim should be aware of where the eyewash stations were located and flush the eyes, nose, and mouth with copious amounts of water. But running from the OR or ICU to the eyewash stations in the lab is often not a practical option. Imagine holding a bloody towel over your face and eyes while running down the hospital corridor and trying to keep dripping blood from contaminating the floors, doors, and even the elevator.
What Are The Risks?
Epidemiologists claim that the risk of acquiring an infection by blood contact with the face and eyes is a remote possibility. That may be true, but there is still a risk. I once heard an investigator for the National Transportation Safety Board say that “remote possibilities happen all the time” about aviation accidents (a valid but oxymoronic statement if ever there was one). And there is no data on how many perfusionists get blood born infections at work. I was seriously infected by an accidental needle stick back in the 1970s. It took me nine months to recover, and I have lifelong ramifications associated with that infection. So, I am gun shy when it comes to blood-borne infections.
What Is The Worst Thing?
The worst thing about gross blood to the face is the fear and emotional trauma the victim experiences. Whenever a person’s face is grossly splashed with another person’s body fluid, including blood, there is often an immediate revulsion. Whenever such a thing happened, I saw perfusionists and other healthcare workers gag, freeze with shock and even cuss loudly. But the one thing all these victims have in common is the intense and immediate desire to wash their face, mouth, nose, and eyes. Nobody completes a case with a grossly bloody face if they can help it. Things can be worse if there is no qualified person available to relieve a bloody comrade. Just wiping one’s face with a towel will not reduce the revulsion or the risk.
A Traumatizing Experience.
This traumatizing experience is not even recognized as such by OSHA, JC, CMMS, or AORN. If someone is verbally abused on the job, that is recognized as workplace trauma, but a face full of blood, no (1). Ever have a surgeon yell or even scream at you? Just try working with a face full of blood. I’d rather have the yelling and screaming. Then there are the privacy issues that may arise if the facility requires the patient and perfusionist to undergo HIV, HBV, and HCV testing. Eyewash stations won’t prevent that. I am just trying to illustrate the compounding traumatizing effect such an incident can have.
What Health Care Workers (HCW) Are Exposed?
By far, HCW with percutaneous (sharps) exposures are at greatest risk for a blood-borne infection, and this includes perfusionists. However, perfusionists, ECMO specialists, and hemodialysis nurses and technicians are the only healthcare workers that I know of that routinely operate equipment containing a large amount of blood under pressure that can suddenly and accidentally escape directly into their face. But anyone working in the OR could be at risk. One of my favorite compositions is a story about Bloody Brenda, an OR nurse who was literally drenched, head to foot, in blood in an OR without adequate protective clothing or emergency washing facilities (2). What about lab people? They are exposed to blood. But the volumes they are exposed to exceed 10 mls rarely, and it is only under pressure when it is in a centrifuge. Besides, labs are required to have eyewash stations close by for other reasons. We need them close by our work areas as well. A failure modes and effects analysis I posted can be found here on the AmSECT Safety page: FMEA # 43 Failure to prevent gross blood to the perfusionist’s face. https://www.amsect.org/page/fmea-archives .
Addendum: OSHA, JC, And ANSI Eyewash Standards
OSHA Eyewash Standards
The OSHA requirements for emergency eyewashes and showers, found at 29 CFR 1910.151(c), specify that “where the eyes or body of any person may be exposed to injurious corrosive materials, suitable facilities for quick drenching or flushing of the eyes and body shall be provided within the work area for immediate emergency use.” As the standard states, an eyewash and/or safety shower would be required where an employee’s eyes or body could be exposed to injurious corrosive materials. If none of the materials used in this work area is an injurious corrosive [chemical] (as indicated by the Material Safety Data Sheet (MSDS) for each product), then an emergency eyewash or shower would not be required pursuant to 1910.151(c).
https://www.osha.gov/laws-regs/standardinterpretations/2009-06-01
JC Eyewash Standards
The Joint Commission references American National Standards Institute (ANSI) Z358-1 as a basis for evaluating eyewash station and emergency shower design configurations and functionality. The need is based on the corrosive level noted of the material being handled and the risk of exposure. However, a proactive, defensible, documented risk assessment process that may deviate from Z358.1 is acceptable provided OSHA criteria is not compromised. Eyewash bottles are acceptable as supplemental devices to eyewash stations (cannot replace) and should be employed through the risk assessment process for applicability.
https://www.jointcommission.org/standards/standard-faqs/hospital-and-hospital-clinics/environment-of-care-ec/000001233/
ANSI Eyewash Standards
While not having the force of a regulation under the OSHA Act, the current American National Standards Institute (ANSI) standard addressing emergency eyewash and shower equipment (ANSI [Z]358.1-2014) provides for eyewash and shower equipment in appropriate situations when employees are exposed to hazardous materials. ANSI’s definition of “hazardous material” would include caustics, as well as additional substances and compounds that have the capability of producing adverse effects on the health and safety of humans. ANSI’s standard also details the location, installation, nature, and maintenance of eyewash and shower equipment. You also may wish to consult additional recognized references such as W. Morton Grant’s Toxicology of the Eye (Charles C Thomas Pub. Ltd., 4th edition, August 1993) when considering potential chemical exposures to the eye and the appropriateness of installing eyewash facilities to protect employees against hazards associated with particular chemicals and substances.
https://blog.ansi.org/2018/07/emergency-eyewash-station-shower-ansi-z358-1/#gref
