Why Do We Wash The Blood Prime in the ECMO Pump? Nobody Else Does!
The initiation of CPB or ECMO results in the rapid exchange of blood at the rate of 100 ml/kg/min in infants. Cardiac arrest from the rapid infusion of PRBC is a well known complication of blood transfusions. Other electrolyte imbalances can cause cardiac arrhythmias and ventricular over distention. Brain damage and increased mortality from hypernatremia in children is also well documented. The transfusion of PRBC stored in preservatives is not recommended in amounts greater than 15 mL/kg/dose in infants because of the potential adverse effects that these preservatives can have. Yet annually 50,000 children undergo CPB and 3,000 undergo ECMO by being placed on pumps that contain hyperkalemic, hypernatremic and hyperosmotic primes with AS-1 or AS-3 preserved PRBC at the exchange rate of 100 ml/kg/min in infants. Some of the many complications of CPB and ECMO probably are masked by the assumption that they are caused by an unavoidable systemic inflammatory response or unfortunate anticoagulation side-effects rather than by an iatrogenic process that can be mitigated by washing the blood prime.
Virtually no research has been done since 1953 to determine if an unwashed blood prime is safe. Drs. Naomi Luban, Ronald Strauss and Heather Hume (nationally known experts on pediatric blood transfusions) in 1991 and again in 2003 recommended avoiding the use of entire units of PRBC in extended-storage media in massive exchange transfusion, cardiac surgery, and extracorporeal membrane oxygenation in children (1). Under these circumstances they recommended that the preservative medium should be removed and the PRBC re-suspended in an appropriate fluid. In other words the prime should be washed. Their recommendations were “based on calculations and hypothetical settings, not actual data. Accordingly, they are tentative and should be altered as definitive information becomes available.”
Back in the late 1980’s we would prime our pumps, both the cardiopulmonary bypass (CPB) pump and the ECMO pump with a unit of whole blood (WB) and a unit of packed red blood cells. The issue frequently seen at that time was a greatly elevated glucose of the blood prime; frequently higher than a glucometer could measure. This was not good for the patients, particularly the infant and small child. So in the early 1990s, after hemoconcentrators became available, we began ‘washing’ the blood prime in our CPB pumps. We would simply add additional crystalloid fluid to the prime and then remove it by ultrafiltration, diluting the glucose to an acceptable level. This was easy to do on a CPB pump, but we didn’t know how to do it on the ECMO pump prime. So for years the ECMO patients were often subjected to greatly elevated glucose values the first day or two of ECMO.
During the time frame of 1987 to 1995, the types of blood products given to us to prime our pumps changed. First, WB no longer became available, only citrated PRBC and fresh frozen plasma (FFP). Then by 1995 mostly AS-1 PRBC and FFP were available. As the blood products changed so did the amount of acid in the PRBC. WB retains much of it natural buffers. So to adjust its pH to a compatible 7.4, only a small amount of NaHCO3 needs to be added. When the plasma is drawn off to make citrated PRBC, most of the natural buffers are removed and the acid builds up in the PRBC. This requires the addition of larger amounts of NaHCO3 to normalize the pH. With AS-1 PRBC any residual natural buffers are totally removed and the acid needs lots of NaHCO3 to be normalized.
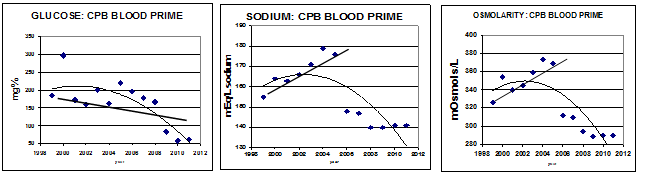
Beginning in the mid-1990s we began to notice more frequent complications of edema and renal insufficiency in the post-CPB patients. By 2005 the situation had become intolerable with the surgeon becoming quite vociferous with his complaints about post-op edema and renal dysfunction. While we were doing a good job of controlling elevated glucose values the sodium and osmolarity of the CPB pump prime were well above the normal range. See the graphs below. From 1999 through 2005 the sodium of our CPB blood prime rose from 155 mEq/L to almost 180 mEq/L (normal = 135-145). As the sodium increased the calculated osmolarity also increased from about 325 mosmols/L to 370 mosmols/L (normal = 270-300). See the graphs below.
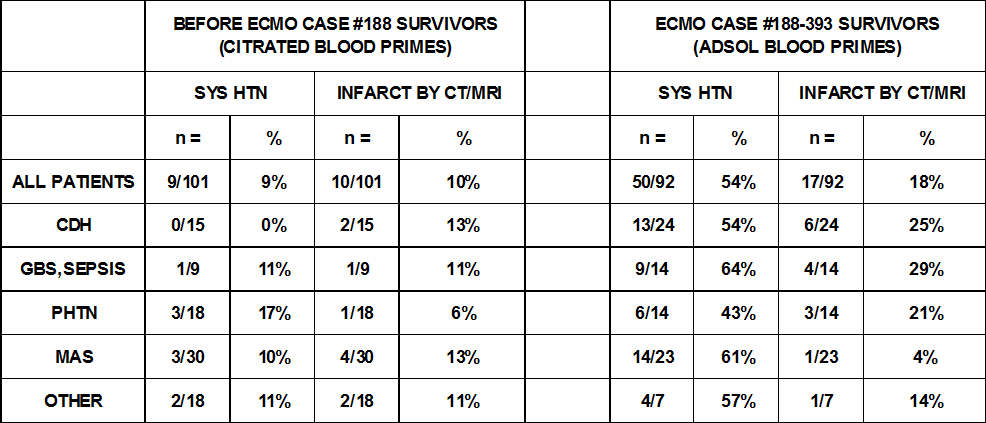
We were seeing changes in our ECMO patients as well. Prior to Nov of 1995 (ECMO patients 1-188), only 9% had systemic hypertension requiring treatment and the brain infarction rate was 10%. After Nov. 1995 through Sep. 2005 (ECMO patients 189-393), 54% had systemic hypertension and 18% had brain infarcts. See the table below.
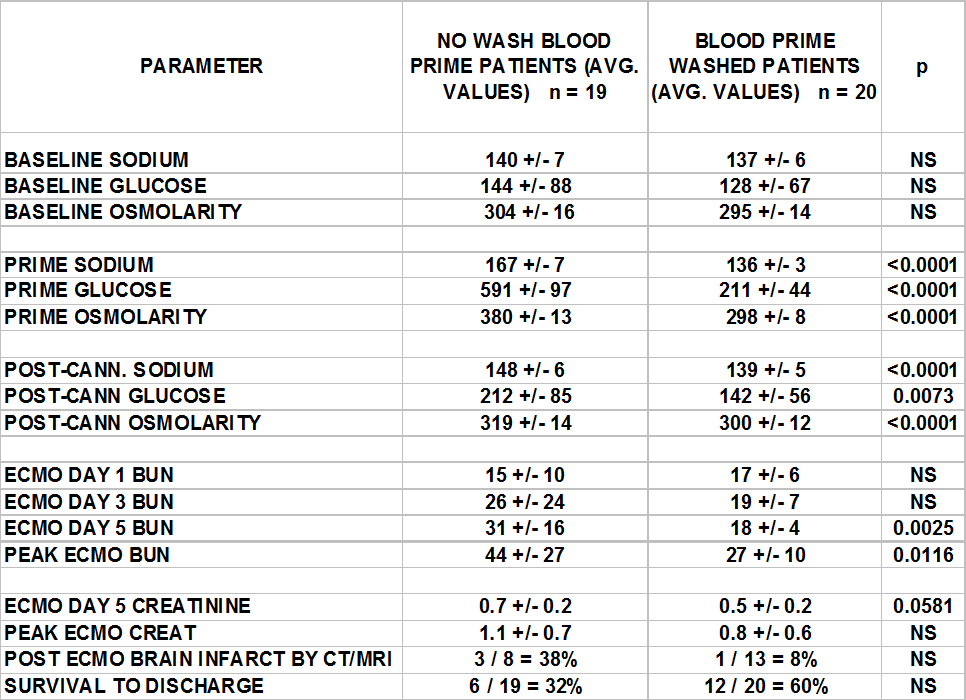
At that time a review of the ECMO pump primes and post-ECMO labs of the most recent 19 ECMO patients demonstrated hypernatremia, hyperosmolarity and renal dysfunction. A prime wash process was instituted in an attempt to mitigate these abnormalities in the prime. These last 19 patients with unwashed ECMO blood primes were compared to the succeeding 20 ECMO patients who received a washed ECMO blood prime after prime washing was formally instituted. See the table below.
Both the CPB and ECMO patients were suffering from the need for excessive amounts of NaHCO3 in the prime to normalize the pH. So in 2006 we modified our wash techniques to better control the prime sodium and osmolarity. And, for the first time, we began washing the blood prime of the ECMO pump in a fashion similar to that used for our CPB pump. We were successful in lowering both the sodium and osmolarity. Many of the complications we had been seeing were becoming much less frequent.
So why don’t other people wash their blood primes? Well, some do. About half of the pediatric perfusionists wash their CPB blood primes. The other half thinks that the edema and renal complications are the result of an unavoidable systemic inflammatory response syndrome seemingly associated with extracorporeal support and that washing is just a waste of time. Most ECMO program primers don’t know about the problems caused by hypernatremia and hyperosmolarity, again thinking that these complications are just part of the normal risks of going on ECMO.
When a baby is first placed on ECMO without washing the prime there are outward signs that things are not right. But since the child is covered by sterile drapes during the cannulation surgery and the outward symptoms resolve fairly quickly, nobody notices. But when an ECMO circuit is changed to a new circuit with an unwashed blood prime and the child is no longer hidden by sterile drapes the child can exhibit some startling symptoms. Among the symptoms I have seen are sudden and severe Harlequin sign, vasodilation of the entire skin surface causing the child to turn beet red, seizure-like movements, hemodynamic instability, cardiac arrhythmias and pulmonary hemorrhage. Delayed symptoms include renal dysfunction and brain hemorrhage or infarct.
The ‘Harlequin sign’ in newborns is thought to be a benign and temporary imbalance in the tone of cutaneous blood vessels secondary to hypothalamic immaturity with no known pathologic significance. However, ‘Harlequin syndrome’, which looks very similar, is caused by damage to the autonomic nervous system. This may be a symptom of injury to the central nervous system caused by the sudden infusion of a large amount of unwashed pump blood prime.
Two years ago an out of town ECMO transport team came to take one of our infant ECMO patients to a distant city for further treatment. The perfusionist priming his portable ECMO pump with PRBC infused NaHCO3 in an amount I would consider too high. He also added mannitol which further increased the osmolarity to a level that I would consider dangerous. But he reassured me that he was following their normal prime procedure. Upon transferring to this new ECMO circuit from ours, the infant exhibited the most profound Harlequin sign that I had ever seen; completely beet red on the left side and blanched white on the right side with a precise line of demarcation from the top of his head to his pubis. The peds physician on the transport team was quite alarmed at this. But in my experience this was a common occurrence in infants when exposed to an unwashed ECMO circuit prime. Two days after arriving at the new hospital the child demonstrated a brain hemorrhage and infarct by CT scan. The patient expired. Was this co-incidence or did the unwashed blood pump prime play a part? I think it did. So that’s why we wash the blood in the ECMO prime.

How are you doing this washing on the ECMO pumps specifically ? Thanks G. Coates
Gary, I will send the procedure with all the specifics to your e-mail address. But, in a nutshell, we placed a small hemofilter in a shunt between the post oxygenator arterial line and the pre-pump venous line. This is the shunt we used to power the CDI monitor. The entire circuit was primed with saline. During blood priming, we displaced the saline with 1u PRBC and 1u FFP. With the sweep gas on and the sweep gas CO2 adjusted to approximately 5% CO2, the blood was recirculated. The AV loop was partially clamped to help push blood thru the shunt/hemofilter. At the same time we shuttled a balanced electrolyte solution thru the bath compartment of the hemofilter. The blood passing thru the hemofilter would adjust to the “wash” solution which had a perfect balance of electrolytes, including HCO3. In this way we were able to adjust the blood perfectly without causing a high Na and high osmolarity that often occurs if NaHCO3 is added directly to a blood prime to adjust the pH. The wash solution also reduces the glucose in the blood prime, further improving the osmolarity.
This is really interesting. We here in serdang general hospital are providing ecmo for both paeds and adult cardiothorasic patients. We would definitely would like to try your methods. Since we also do have the same issues with using prbc during cpb n ecmo, we would try to use this method. Tq.
Vicky- If I can be of any assistance you can contact me at garygrist@comcast.net.
-Gary
Hi Gary,
I know this is an older post, but I was hoping that you might still be willing to share your washing procedure for reference. We do wash our ECMO primes for Peds, but are still adding in medications as we are doing it. I’m hoping to update and improve our process. Thank you!
Jamie-
You are welcome to use anything you find on the Perfusion Theory web site for reference. If I can be of any further help please let me know.
-Gary
Hi Gary,
We blood prime for our ECMO patients that are less than 10 kg. We have adjusted the medications over time that we add to our blood prime, but this is the first I have heard about ‘washing’ ECMO primes and would really like to hear more about this, if you would be willing to share. Thank you!
Jeliene-
Experience and close observation taught me that most of the deaths on ECMO are caused by reperfusion injury due to placing the patient on ECMO too late (1,2). You should also read this article: https://perfusiontheory.com/oxygen-pressure-field-theory/session-4-breaking-the-reperfusion-barrier-perfusions-21st-century-challenge/ . However among neonates and infants there is a high mortality from brain hemorrhages in particular. Although this can be aggravated by reperfusion injury, these brain hemorrhages are caused by an improperly primed pump.
The article describes how the osmolarity of the prime can be greatly elevated by NaHCO3 added to the prime and the glucose already in the bank blood. Since the prime volume in neonates and infants is quite large in comparison to their own blood volume, this results in a sudden and drastic change in blood osmolarity when the pump is started. This sudden change in osmolarity can damage the fragile and immature blood vessels, especially in the brain.
Calcium is also a great mediator of reperfusion injury. If calcium is not added to the blood prime to counteract the citrate in the blood, the heart may actually stop. Washing the blood also removes much of the citrate and other preservatives in the bank blood which are hazardous in small patients when the blood volume is suddenly exchanged. A normal blood transfusion usually takes 4 hours as recommended by AABB for safety reasons even in adults. But on pump even if started slowly, the exchange transfusion takes only a few minutes and sometimes only seconds. If extra calcium needs to be added to the prime to counter act the citrate, this can further aggravate reperfusion injury. Washing helps to remove the blood citrate so that only small amounts of calcium gluconate need to be used, totally eliminating the need for CaCL2 which is an extremely dangerous and caustic medication.
So I think it is important to wash the blood in both ECMO and CPB pumps when using a blood prime on small patients. When I say “wash the blood” I am referring to using a hemoconcentrator and specially mixed IV solutions with NaHCO3 added so that it does not exceed 300 mOsm. The excess fluid is removed by the hemoconcentrator to also reduce the glucose, citrate and preservative levels in the prime. Most pediatric perfusionists perform some type of washing when priming a CPB pump with the goal of keeping the blood prime osmolarity <300 mOsm. A blood osmolarity of 320 can precipitate renal failure and an osmolarity of 370 can cause permanent brain damage.
When you prime your ECMO pump you should measure the osmolarity of your prime. If it is less than 300 mOsm, then you don’t need to wash it. But if not, you should find a way to reduce the NaHCO3, glucose and CaCl2 in the prime. I would be happy to send you my washing procedure for an ECMO pump prime. Contact me at garygrist@comcast.net .
1) Grist G, Whittaker C, Merrigan K, Fenton J, Pallotto E, Lofland G. Defining the late implementation of extracorporeal membrane oxygenation (ECMO) by identifying increased mortality risk using specific physiologic cut-points in neonatal and pediatric respiratory patients. J Extra Corpor Technol. Dec 2009;41(4):213-219.
2) Grist G, Whittaker C, Merrigan K, Fenton J, Pallotto E, Molitor-Kirsch E, Ostlie D, O’Brien J, Lofland G. Identifying Neonatal and Pediatric Cardiac and Congenital Diaphragmatic Hernia Extracorporeal Membrane Oxygenation Patients at Increased Mortality Risk. J Extra Corpor Technol. Sep 2010;42(3):183-190.
What about in cases of ECPR? Is your center able to get blood washed fast enough to use it in a cardiac arrest setting? If not, how do you modify your protocols in the setting of emergent rapid deployment
Kiona-
We did not wash the blood for ECPR. We always used a room temperature clear prime designed to immediately cool the patient. For ECPR patients under 6 kg we had a special circuit using a 40 ml oxygenator and low volume circuitry (3/16) and a peds c-pump and no other bells or whistles. Once we got the patient stabilized in a matter of hours we would put them on a blood primed circuit before rewarming if needed.
Most of our ECPR patients were over 6 kg and could tolerate a clear prime with hypothermia on our regular pediatric ECMO circuit.
The physiology of ECPR is completely different than the physiology of ECMO. This article will explain the difference and how initiation of ECLS needs to differ between ECPR vs ECMO. https://perfusiontheory.com/oxygen-pressure-field-theory/session-4-breaking-the-reperfusion-barrier-perfusions-21st-century-challenge/
Thanks for the question.
https://perfusiontheory.com/oxygen-pressure-field-theory/session-4-breaking-the-reperfusion-barrier-perfusions-21st-century-challenge/
Extremely interesting article with profound points regarding the physiologic aspects and effects of ECPR and placing these patients on support emergently. I would be interested to know how many other centers have included aspects of these management techniques within their programs. Very informative article in relation to ECPR and reperfusion injury. Thanks for posting.