The Tale of Bloody Brenda: A Tribute to OR Nurses By Gary Grist RN CCP Emeritus
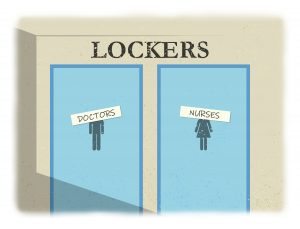
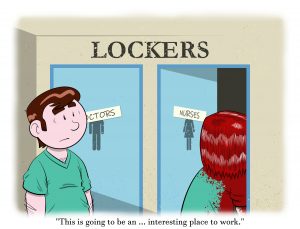
Many decades ago, I walked into the new hospital operating room where I was just hired as a perfusionist and a scrub nurse. Two of the first things I saw were the OR locker room labels; “Doctors” and “Nurses”. I immediately thought that this was going to be an interesting place to work. Since I was a scrub nurse I assumed I would be in the “Nurses” locker room. I was one of the very few male nurses in the hospital and the only one in the OR. But I was directed to the “Doctors” locker rooms. The signs should rightly be interpreted as “Men” and “Women”, I was told by my supervisor, who apparently did not recognize the offensive nuance of the labels. In fact, there were no female physicians working in the OR; neither surgeons or anesthesiologists. However, there were two excellent nurse anesthetists who bunked on the “Nurses” side.
by Jimmy Grist
That wasn’t all. Both locker rooms had the same number of lockers, which seemed fair at first sight. Except that there were four times more “Nurses” than “Doctors”. So each physician got his own locker but the nurses had to double up or even triple up. Also, the “Doctors” had a shower and the “Nurses” did not. Whoever designed these locker rooms apparently did not think that OR nurses would get sweaty and bloody during the work day and might want to shower off before going home. Apparently, getting sweaty and bloody only applied to “Doctors”.
“Doctors” wore the typical scrubs that we all wear today; a pullover shirt and pants with a cord waist tie. The “Nurses”, however, were REQUIRED to wear these horrible short sleeve scrub dresses. They hated them for too many reasons to expand upon here. The hospital did not even supply them with warm up jackets. The nurses could buy their own jackets, but they were required to be freshly laundered every day. The nurses were not allowed to wash the jackets at home. They must use the hospital’s outside laundry service where they could be properly sanitized. After two or three runs though the outside laundry, each nurses’ own jacket was usually lost (or maybe stolen) by the outside contractor /:= ( When they were not scrubbing many of the nurses took to wearing our re-useable, sterile cloth (yes, I said cloth) scrub gowns for warmth and arm protection. This was frowned upon by the powers-that-be because it used the sterile gowns for a non-sterile purpose causing the labor to repair (patch holes), launder and sterilize these gowns to go to waste. (Was it wasteful to want stay warm and clean from patient detritus? I didn’t think so!) Even though I was a scrub nurse, I was also a perfusionist. So I guess it was OK for me to wear pants and shirt.
These are just some of the examples of what the nurses had to put up with in the late 70’s and early 80’s. Actually, things had improved some since I started working in the late 60’s. Back then, floor nurses were REQUIRED to wear their nursing caps, as well as white dresses or white skirts and blouses with white hose and white shoes. As I remember, “Doctors” had no dress code. The 60’s was a time in American medical culture when doctors were treated like gods and nurses like handmaidens. And the most godly “Doctors” of them all were the heart surgeons. Nurses were expected to stand and offer up their chair whenever a surgeon came on the floor or entered an operating room. (I am not kidding about this!) And if a nurse or any other paramedic were to offer advice to any doctor, they were considered “uppity and disrespectful”. It could even cost them their jobs if the doctor complained to the hospital administration.
At least, in the late 70’s and early 80’s, nurses no longer had to stand when a doctor (particularly a surgeon) entered the room. And it was a lot harder for doctors to have a nurse who they did not like fired. Nurses still showed physicians respect, but they no longer showed the deference of a servile handmaiden *. As one popular cigarette commercial of the time said; “You’ve come a long way, baby!”
That brings me to Brenda. Brenda was a scrub nurse (RN) who scrubbed mostly hearts. I worked with her most days. When not scrubbing hearts, she scrubbed every other thing that came down the pike; ortho, ENT, neuro, eyes, etc. Brenda was absolutely dedicated, as most of the OR nurses were, to helping sick kids in any way she could. Even if it meant putting up with the abusive and disrespectful nuances within the OR environs.
One day a severe trauma patient arrived. This was a girl about 10-12 years old who had been in an auto accident. Her pelvis was crushed and she was bleeding profusely from her perineal area. The pelvis is made up of seven large bones fused at sutures in childhood. If the suture fusions are ruptured or the pelvic bones themselves are broken open, bleeding becomes a serious problem. This is because the pelvic bones are the largest flat bones in the body and contain a lot of bone marrow. They also act as reservoirs for venous blood. If a pelvic bone is fractured, the internal bleeding can be as bad as if the inferior vena cava is severed. This child also had perineal trauma and the prolific bleeding from the crushed pelvis was coming out of that wound.
We rushed into the OR and positioned the child on the table. Brenda donned a mask and gloves, grabbed some large lap sponges and applied pressure to the perineum to try to stop the bleeding. When the orthopedic surgeons (pods) came into the room, they had us lower the foot of the table and attach knee crutches to hold the child’s legs in a ‘knee and hip’ flexed position. Brenda kneeled at the foot of the shortened bed, still pressing the lap sponges against the torrent of blood.
The surgeons and two scrub nurses quickly gowned and gloved (there was no time for a proper hand scrub). They threw some betadine over the child’s lower abdomen and hips followed by the positioning of a large sterile surgical drape which covered the whole child, the entire table ….. and Brenda. They then proceeded to do something I had never seen before or since. They used hand drills to make holes on either sides of the child’s pelvis. Then they endeavored to feed a rigid steel rod through the hole on one side, trying to avoid other vital pelvic organs and structures, through to the other side. The idea was that once the rod was through-and-through the pelvis, they could apply washers and nuts on each end of the rod. As the nuts were tightened, the squeeze from the washers compressed the pelvis and its ruptured boney sutures together and, hopefully, stop the bleeding.
What was everybody else doing? The anesthesiologist was busy establishing a secure airway, starting large bore IV access, giving anesthetic medications, monitoring and charting vital signs (this was well before computer charting, automated blood pressure cuffs and even pulse-oximeters) and reversing the shock that was rapidly developing.
The scrub nurses were trying to pass the surgical instruments and keep their Mayo stands organized as the surgeons kept lobbing instruments back at them in a frenzy.
My job was to pump blood in. There was no cell salvage in those days. There were no packed cells then either. We used whole blood. I went through the first few units of cross-matched, type specific blood that we had. That was gone in about 5 minutes. Then I began to give just type specific blood. When we ran out of that, I started pumping in type compatible blood. We rapidly depleted most of the blood in our in-house blood bank. The community blood bank was rushing more units to our hospital. I don’t remember exactly, but I think I eventually pumped in about 50 units of whole blood during the procedure.
The circulators were charting and running for supplies, particularly large lap sponges. Then I suddenly thought, “Hey! Where’s Brenda?” The last time I saw her, she was kneeling at the foot of the bed still trying to stem the flood of blood with a lap sponge. She was still there, throwing out blood soaked (and I mean SOAKED) sponges and yelling for more! She remained there though out the case, on her bare knees, in that lousy scrub dress. The only protection she had was her bouffant hat, paper face mask and rubber gloves. No gown and no eye protection.
I yelled for somebody to relieve Brenda. But she wouldn’t hear of it. She was already contaminated from multiple units of donor blood flowing from the wound; on her head, face and eyes, down her bare arms into the shoulder openings of her dress and over her bare, unprotected legs. She did not want anyone else to risk a similar exposure. In fact, there WAS NOBODY free to relieve her. All the OR personnel were already tied up in this case or in other on-going cases.
Finally, after about 45 minutes, the pods succeeded in ratcheting the nuts and washers tight enough against the sides of the pelvis to close the fractures and stop the bleeding. I could not believe it worked! Frankly, I don’t think the pods believed it was going to work either.
When the drapes came off, there was Brenda still holding pressure against what was now a trickle of blood. As she stood erect I could see that she was covered in blood, from head to toe. I had never seen a human being bathed in blood like she was; but she was beautiful for what she did.
We managed to get the patient out of the OR alive, but I do not know if the child survived to go home. I don’t think it was possible, but you never know. I have seen some genuine miracles in my time. This could have been one.
Some of the other nurses helped “Bloody Brenda” to the “Doctors” locker room where she got in the shower to wash the gore off. Her clothes, including her underwear and OR shoes were discarded in the contaminated waste. There was no hope of saving them. She drove home in one of those terrible scrub dresses (to protect her good street clothes from any residual blood and germs) and her street shoes. Once at home, she soaked in a tub and washed her hair with her own shampoo to soak off the musty, rancid smell of shed blood.
by Jimmy Grist
Brenda was not any more dedicated than any of the other wonderful OR nurses I worked with. In fact, she was typical of them. Anyone of those nurses would have done the same if they had been in the same predicament. If not for Brenda’s action to stifle the blood flow, I am certain that child would have died in the OR during surgery. I am proud to say that I worked with Brenda and this extraordinary group of “uppity and disrespectful” OR nurses.
Post script: The battle of the scrub dresses was soon to end. One of the “pro nurse” anesthesiologists began wearing scrub dresses while he worked to make a point. I think it made the other doctors uncomfortable to see his hairy legs. Soon the policy mandating scrub dresses for female nurses was modified. The hospital would still have scrub dresses, but now the nurses could wear “womens” scrub pants. These were almost as bad as the dresses. These scrub pants were the kind with a wide elastic waist band and extra-wide hip room; essentially “maternity” pants for OR nurses.
Soon both the dresses and the maternity pants started to disappear. I blamed the outside laundry service 😉 With the scrub clothes shortage, the nurses were forced to wear “Doctors” scrub clothes or they couldn’t work. The hospital kept buying replacement dresses and maternity pants, but they mysteriously kept disappearing. Soon it became a matter of financial stress on the OR operating budget to constantly replace the dresses and maternity pants. So the OR nurses were finally allowed to wear the more comfortable “Doctors” scrubs. Not too long after that, the nurses got warm up jackets and a shower in their “expanded” locker room with additional lockers. Was Bloody Brenda’s adventure responsible for all that? I say definitely “Yes”…… possibly.
What happened to Bloody Brenda? She went back to school and became an excellent and well respected nurse anesthetist specializing in pediatrics. Perhaps she wanted to work at the head of the table rather than under it!
*“The Image of Nursing: The Handmaiden”, author Sandy Summers. Nursing Times. Oct 7, 2010. https://www.nursingtimes.net/roles/nurse-managers/the-image-of-nursing-the-handmaiden/5020163.article
