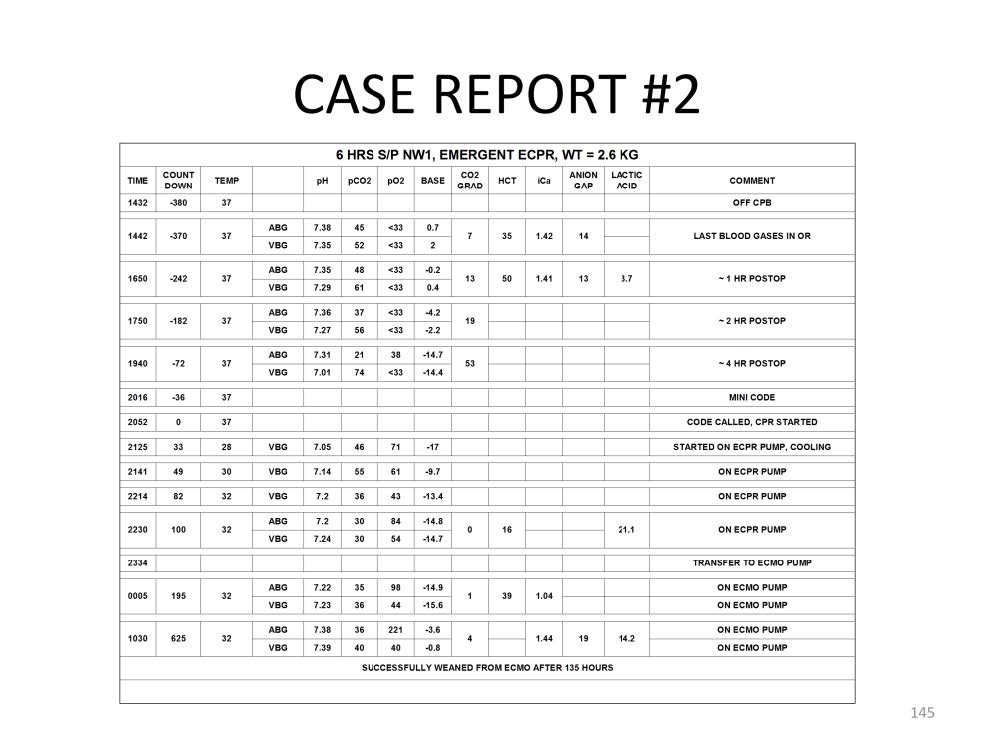
In this case report a 2.6 kg infant underwent a Norwood stage one procedure for hypoplastic left heart syndrome. The time till cardiac arrest is represented as a “count down”. The last set of blood gases (ABG and VBG drawn at the same time) in the operating room document normal values with the exception of low pO2 values. These are normal pO2 values for this type of mixing lesion. The p[v-a]CO2, the hct, the iCa and the anion gap are all normal at T minus 370 minutes till arrest. At T minus 242 minutes, the p[v-a]CO2 increased to 13 mmHg and the lactic acid was slightly elevated at 3.7 mmol/L. The patient received a blood transfusion to increase the hct to 50%. At T minus 182 minus, the p[v-a]CO2 increased to 19 mmHg and a base deficit was beginning to develop. In retrospect, the frequency of lab analysis should have been increased at this time to at least every 60 minutes and serious consideration should have been given to starting VA ECMO. At T minus 72 minutes, the p[v-a]CO2 was 53 mmHg and the base deficit increased to -14 mEq/L, prompting a call to the surgeon suggesting the implementation of ECMO. Before ECMO could be started, the patient arrested 380 minutes after coming off CPB. After 33 minutes of CPR the patient was placed on ECPR and cooled to 28C and the hct dropped to 16%. Over the next 100 minutes of ECPR the patient’s temperature was stabilized at 32C and the venous pH and pvCO2 were normalized. The patient was transferred to a regular ECMO pump and the hct normalized. The patient’s iCa was normalized 625 minutes after arresting. The patient spent an additional 125 hours on ECMO, followed by successful weaning and discharge from the hospital without detectable cardiac or CNS morbidity.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.