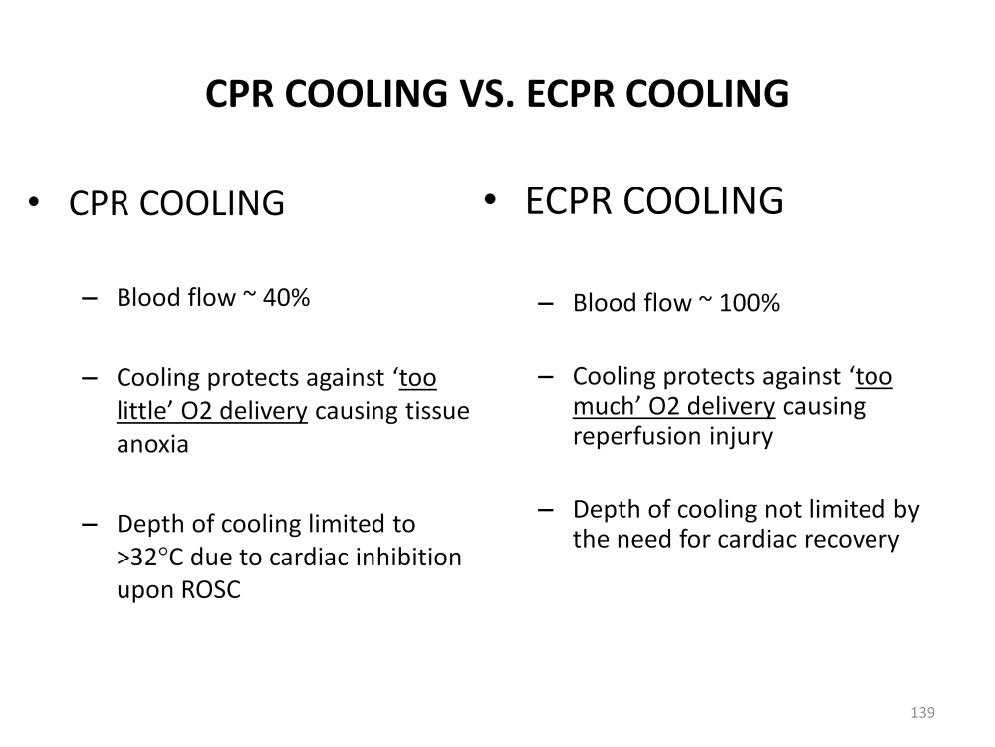
There is a difference between the need to cool a patient during conventional CPR and cooling when placed on ECPR. During resuscitation CPR the best blood flow to the brain that can be expected is about 40% of normal. However, once ECPR is started, blood flow approaching 100% of normal can be expected.
Cooling during CPR is performed to protect the organs from ‘too little’ O2 delivery by reducing the metabolic need for oxygen. Paradoxically ECPR cooling is needed to protect against ‘too much’ oxygen being delivered by the pump. Providing enough pump flow to maintain blood pressure will simultaneously deliver copious amounts of oxygen from the oxygenator compared to CPR even if a 21% FiO2 sweep gas is used. This will cause reperfusion injury in a patient with RIP. Hypothermia is the only proven clinical treatment to prevent reperfusion injury from this over oxygenation by the pump.
During CPR, cooling is limited to no less than 32-34°C. If the heart gets too cold, it may not adequately support a patient’s hemodynamics upon ROSC. A recent trial of targeted hypothermia (33°C) used in pediatric brain trauma patients without cardiac arrest demonstrated significantly more hypotension and increased need for vasoactive agents than their normothermic counter-parts with almost twice as many deaths in the hypothermic group. This may have been related to poor cardiac function during hypothermia and the subsequent rewarming. However since cardiac function and ROSC are not primary concerns once ECPR is started, hypothermia need not be strictly limited.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.