Past VI – Dr. Walton Lillehei’s Second Plan – Standing on Tall Shoulders – The History of Cardiac Surgery by Thomas N Muziani PA-C, CP
“The Pendulum of the Mind Oscillates between Sense and Nonsense- Not between Right or Wrong” Carl Gustav Jung
Walton Lellehei had become exceedingly cognizant of the general mood displayed by physicians and researchers proclaiming “we have progressed as far as we could possibly go” when discussing repairing the mal-formed congenital human heart. This on-going ill informed vitriolic diatribe was entering its seventieth year. One of the real benefits of practicing medicine in general, and surgery in particular, in the Midwest and West Coast of the United States was the fact that distance seemed to provide amnesia.
However after Dr. Lillehei’s first 45 patients were operated on utilizing cross-circulation to facilitate performing the repair he felt compelled to write: “The demonstration that right ventricular cardiotomy and septal suture can be successfully performed even in seriously ill patients should dispel much of the discouragement previously prevalent in this field and stimulate further rapid developments in the application of direct vision intracardiac corrective surgery to congenital and acquired cardiac pathology” .
Walton Lillehei’s Second Plan Takes Root
The obligations of the operating room were demanding more and more of Lillehei’s time. His love of research would be placed on hold and relegated to his devoted and ever inquisitive young associates; Morely Cohen and Herbert Warden. Both Cohen and Warden were very active and quite content performing heart operations on animals in testing procedures for human use. As fortune would have it, a young physician with a “very pregnant” wife found it mandatory to carve out a new niche for himself in medicine. Dr. Richard DeWall, in the hope of securing a job, decided to take a model of a mitral valve he carved from Plaster of Paris to his former instructor Dr. Richard Varco at University of Minnesota Medical School. Varco realized very quickly that DeWall displayed a unique talent in biomedical research and the capacity to function with minimal supervision. He decided to encourage and promote that talent.
As Dr. DeWall would later write: “Dr. Walt Lillehei had a research lab in the basement. Although the lab’s budget had no line item for a research assistant, Lillehei could pay me as an animal attendant”. “I just got the dogs out of the cages and set them out for surgery”.
During this period of the early 1950’s, rubella, also known as German measles, became a major epidemic coinciding with the baby boom post World War II. Sick children with Rubella inundated the Emergency Rooms at Minnesota’s largest regional medical center, leaving many of those children with damaged hearts.
While undergoing basic training during World War II, DeWall developed a heart murmur due to an enormous epidemic of scarlet fever at the Great Lakes Naval Station north of Chicago. “I think I went in with a company of 120 men, and only half of them graduated on time. The rest were in the hospital”.
After witnessing a 15-year-old boy in hospital enduring treatment for rheumatic heart disease, DeWall fixated on a basic question: “The heart is fundamentally a pump. Why don’t we just open the pump and replace the valve? Because people have been doing that with pumps for 2,000 years!”
DeWall’s first project was to assist in the development of cross-circulation technique, utilizing a parent to act as the oxygenator with a small pump to facilitate blood flow into the patient… thereby allowing correction of the congenital defect. In the course of 18 months, the team performed 45 surgeries on children…28 patients, or 62%, went home. Of these, 49% were alive 30 years later.
Ninety miles south of University of Minnesota, a clinic that had morphed into a major medical center emerged was founded by William Worrall Mayo in 1864 as a result of his appointment as Examining Surgeon for the military draft board during the Civil War. Rochester Minnesota was a city to his liking. Post World War II, the Mayo Clinic realized that returning GI’s, empowered by the GI Bill, would be looking to resettle into a new, friendly area. Rochester and the Mayo Clinic had great “curb” appeal.
John W. Kirklin, having just graduated from Harvard in 1942 was in search of just such a place. Accepting the position at Mayo with an abundant of funds for both surgery and research, Kirklin approached John Gibbon about the use of his heart-lung machine. The machine had been modified by Dr. Michael DeBakey, who incorporated a roller pump he devised at the age of 23 and Richard (Dick) Sarns, a brilliant engineer. The pump now included tubing guides to prevent tubing kinking and the ability to adjust occlusion of the tubing. The new machine was branded Gibbon-IBM model II. John Gibbon very generously provided the plans to Kirklin free of charge.
Upon viewing the new heart-lung machine at Mayo, Dr. Lillehei realized this could provide the answer he needed. When he returned to University, his one comment to DeWall was: “This would be a good project for you”. Lillehei also provided two admonitions: “Don’t use a bubble system” to oxygenate blood, because it has “a very poor history” and “avoid libraries and literature searches” that could potentially lead DeWall to repeat mistakes made by others.
Over the course of the ensuing months, DeWall became engrossed in the project. It necessitated applying all of his university acumen in flow dynamics, thermal convection, stasis, geometry and medicine. To infuse donor blood with fresh oxygen, DeWall experimented with exposing the surface of blood to oxygen by means of an inclined tube. His empirical knowledge and pragmatic nature suggested he substitute a helix instead of a straight tube. This would allow the same principals to work in a confined space, which would function better in an operating room.
Having almost zero funds available forced him to scavenge for equipment. Lillehei introduced DeWall to a gentleman that was utilizing flexible tubing to pump mayonnaise in a nearby factory. As DeWall would later write: “Fortuitously, the polyvinyl was very much blood compatible.” Prior to this, almost all oxygenators utilized solid glass tubing, which disrupted blood’s capacity to clot, leaving huge fibrin threads and “boogers” (clots) stuck in the tubes. DeWall came to realize there were added advantages to using polyvinyl when he experimented with infusing blood with oxygen under three atmospheres of pressure, enough to enrich the blood plasma itself with oxygen.
The flexibility and strength, coupled with the fact that it was shatterproof, made polyvinyl the ideal vehicle to transport blood. However, there evolved an obvious downside: The increased pressure produced the same unwanted bubbles in blood that divers had to endure if they attempted to surface too quickly to atmospheric pressure. Lillehei’s admonition about staying away from bubbles started to suffuse in his brain.
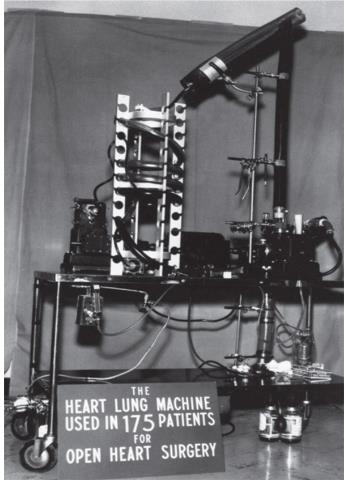
The DeWall-Lillehei Heart-Lung Machine with the DeWall Oxygenator
