Part XIX- Episode 2- Necessity- The Advent of Myocardial Protection- Standing on Tall Shoulders- The History of Cardiac Surgery Thomas N Muziani PA-C, CP
“Nothing has more strength…than dire necessity”- Euripides
“Discontent is the first necessity of progress”- Thomas A Edison
Prologue-
The synergism incorporating hypothermia with cardiac surgery has been described by many investigators as the single most important advance for protecting the heart while operating. Numerous articles have been written about the individual acknowledged as the foremost thought leader in the application of hypothermia – University of Toronto’s Wilfred E Bigelow. In his treatise for the Annals of Surgery 1950 Dr. Bigelow outlined his rationale;
…the oxygen requirements for tissues are reduced to a small fraction of normal…Such a technic might permit surgeons to operate upon the “bloodless” heart without recourse to extracorporeal pumps, and perhaps allow transplantation of organs…Intracardiac procedures upon human beings are heroic technics designed to open a stenosed mitral valve and close or produce a septal defect.”
Beware – the proverbial light at the “end of the tunnel”…just may be a freight train!
Historians credit the birth of modern clinical open-heart surgery to a 1953 article in the publication Surgery by University of Minnesota’s F. John Lewis and Mansur Taufic. The authors wrote about how they drew heavily upon Bigelow’s seminal paper: “Closed under hypothermic inflow occlusion, an atrial septal defect in a 5-year-old child.”
Dr. Wilfred Bigelow
Cardiac surgeons worldwide in 1953 understood immediately the utility of hypothermia. Its inclusion was relatively inexpensive, readily available and cold weather climates provided graphic instinctual comprehension of what cold could create. The empirical experience of applying hypothermia during cardiac procedures deemed it seamless to dovetail the technique with John and Mary Gibbon’s new innovation…the “heart and lung machine with oxygenator”. History will certainly validate this device as one of the greatest inventions for mankind in the 20th Century. Unfortunately there are no tennis shoes, lines of clothing or cologne named for either John or Mary Gibbon.
(GG Note: The American Society of Extracorporeal Technology does give an annual award, the John H. Gibbon Jr. Award, to an individual making a significant contribution to the cardiopulmonary discipline interrelating with the field of extracorporeal circulation.)
The culmination of over two decade’s extensive trial and error performing experiment upon experiment, John Gibbon, along with his wife Mary his assistant and perfusionist, developed a workable heart and lung machine. Dr. Gibbon became the first surgeon to ever successfully apply his new apparatus for the repair of an atrial septal defect; the procedure was carried out on 6 May 1953 on an 18-year-old girl.
In 1955 John Kirklin while at Mayo Clinic reported excellent results with the Mayo Clinic heart-lung machine, designed and built in-house with modifications on the Gibbon apparatus. One of the obstacles they confronted in 1955 was setting and “locking” the occlusion on the roller heads. It is a rather harmless process to pump milk through plastic tubing (the tubing originally utilized was purchased from a dairy). Milk is very forgiving and does not require precision or delicacy in delivery. Blood however, is not very merciful when being mistreated.
Therefore, achieving minimal occlusion with the roller head and preventing it from migrating to a different setting was no small feat. It did not require real effort to over-occlude tubing with the resultant “riding-up” in the roller head eventually bursting the tubing apart. This would provide graphic evidence to the 10th power for the phrase “bloody mess”. Side note; wearing gloves were anathema for perfusion; they were strictly for housekeeping, surgeons and nurses. Another early problem was excessive noise plus heat generated from the wire-wound induction motors. At full flow the machine’s motors sounded and felt as if you were standing next to a massive foundry.
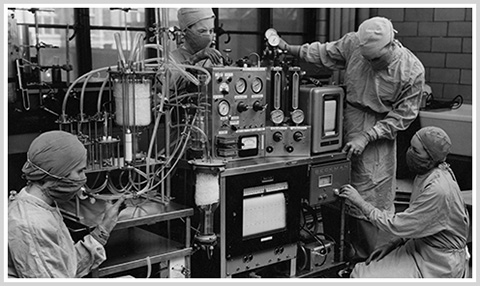
Cincinnati Children’s Hospital– Imagine this for ECMO…on an airplane!
However, with the introduction of extracorporeal circulation, the surgeon was now permitted direct-vision intracardiac surgery…and a whole new set of issues became readily apparent. Within the first operations an obvious concern was dealing with a constantly moving heart and the potential for easily introducing a lethal bolus of air into the heart and/or circulation. Second, the mere complexity of dealing with an object that was constantly moving away from you and trying to sew into that object with suture as thin as a human hair. And finally, with antegrade flow from the coronary sinus and pulmonary veins…coupled with retrograde flow from the pulmonary artery…your operative field was flooded with blood rendering direct vision and repair impossible.
A quiet, bloodless heart and field were an indisputable necessity. However, it is not complex to stop a beating heart…just once and forever! It is a totally disparate mindset to expect that same heart to stop functioning…remain quiet and still…then return to normal- beating, ejecting with force and happy. That requires creativity. The heart must be “fooled” into thinking it is just asleep, never starving for oxygen or devoid of nourishment. The laws of nature and graphic history make it readily apparent that you cannot suspend a human or a duck or a cow, for that matter, by a rope solely around the neck for an hour or more…and then expect that object of divine creativity to come back vibrant and happy. But that’s what this surgery demanded.
While the fledgling cardiac community generally understood that reversible, elective cardiac arrest subjected the heart to pronounced ischemia, surgeons were far more concerned with optimizing operating conditions and minimizing the risk of air embolism. This conundrum created conflict between a surgeon’s demand for concise meticulous anatomical repair and the myocardium’s inexorable requirements for oxygen, blood and substrates.
Professor Denis G Melrose
Denis Melrose while in postgraduate school was confronting this same conundrum. He, along with his colleagues at Royal Postgraduate Medical School, London 1955 were frustrated and perplexed. The conditions of the cardiac patients they had to circumnavigate to repair rheumatic heart valves and avoid air embolism became untenable. Operating on a beating heart going one direction plus constantly expanding and contracting lungs going in opposite directions… to facilitate a repair was analogous to teaching a 5 year old the virtues of Latin as a spoken language.
This prompted Melrose to investigate all nuances of electively instigating quiescence within the heart. In the 2 July 1955 issue of The Lancet, Melrose published his famous study on experimental potassium citrate arrest. His introduction for the article:
“The goal of cardiac surgeons must be the unhurried correction of cardiac abnormalities under direct vision. Toward this end are being developed many techniques for working within the bloodless heart and for excluding the possibility of air embolism after such interventions…A most valuable contribution to this problem of intracardiac surgery would be if the heart could be arrested and re-started at will, suffering no damage during periods of arrest and cessation of coronary blood flow.”
Melrose was very eager to cite the works of Ringer, Hooker and A.V. Montgomery as his primary influences. He described his initial experiments with 33 dogs that had been subjected to either the heart-lung machine or full-body hypothermia. Ligation of the venae cavae, pulmonary artery and aorta excluded blood from the heart.
Diastolic arrest was achieved and maintained for fifteen minutes within five seconds of injecting 25 to 100mg/ml of potassium citrate directly into the aortic root with a syringe. Melrose described that throughout the period of arrest he observed the myocardium remained pink plus serial coronary sinus samples revealed that little if any oxygen was being utilized by the heart. After simulated intracardiac repair, minimal manipulation of the pink flaccid heart obviated air embolism upon closure of the incisional site. Reperfusion with the patient’s own blood in conjunction with cardiac massage…plus the infusion of calcium chloride, adrenaline, and neostigmine were required to restore a normal heart beat.
It was reported that, in almost every instance, ventricular fibrillation resulted upon return of electrical activity. Defibrillating with electrical current was effective only 70% of the cases…and resumption of normal syncopated contraction was not reliable. And yet…unbeknownst to everyone, especially Denis Melrose…the true horrors of this technique had yet to be discovered.

“We Have Met the Enemy! And He is us!”- Pogo-Cartoon character in newspaper comic strips.
