Checklist Errors
Many decades ago, when I first started using checklists, I thought they were an annoyance that just slowed me down. I did not see much value in them. But as I aged I began to realize that I was not infallible. There were many times when I caught myself making errors that a properly structured checklist could have prevented. Fortunately, wisdom often comes with age. I began to see the real benefits of a good checklist. Later, as I instructed students, I realized that a good checklist could help them learn the ropes of the circuit setup rather than just me repeatedly showing them how to setup. I also realized that a checklist that was too vague did not help them much and a checklist that was too complicated just confused them. It is difficult to find a happy medium for students because, unlike staff perfusionists who use the checklist every day for months or years and become very familiar with it, a student must master it in a few days if s/he expects to run the pump during their rotation. This is particularly true in a pediatric program where differently sized and configured circuits are frequently used.
Speaking of becoming very familiar with checklists, I came to realize that familiarity often results in unintentional complacency. Experienced staffers are more inclined to miss or incompletely perform a checklist task because they are working autonomically (like the autonomic nervous system) with very little conscious thought given to each task. It is more of a reflex than a thoughtful action. This can be compared to learning a musical instrument like the piano or guitar. At first it is difficult and deliberate, requiring intense concentration. But later, when mastered, playing the instrument requires very little conscious thought. Proper checklist completion can be further complicated if what little conscious attention being used gets distracted by irrelevant things. This automaticity can be more problematic if a relief perfusionist taking over the setup assumes that the items on the checklist are actually completed when, in reality, they have not been completed.
My solution was to require a double check system. The Amsect Guideline 4.1 states in part: ”Completion of the checklist should be performed by two people, one person being the primary perfusionist responsible for operation of the heart lung machine during the intra-operative period.” That has always seemed to work well for me. Since I implemented double check checklists decades ago, I don’t ever remember spilling the prime because of failing to securely connect a tube, or putting tubing in a pump backwards or not having the sweep gas system work properly when beginning CPB. These errors may be simple enough to correct. But they may be inadequately dealt with by an inexperienced perfusionist or add another layer of criticality in an emergent case.
As I see it, there are four types of checklist errors:
- Action errors occur when a frequent and routine task becomes an autonomic, rote and habitual action that bypasses the active thought process. (If you are an NPR Car Talk fan you are probably familiar with Tom and Ray’s automobile repair suggestions that are: “Unencumbered by the thought process.”) These errors also occur if attention is diverted, resulting in an incomplete or unintended action. These are “slips” (errors of commission, doing something incorrectly) and “lapses” (errors of omission, neglecting to do something).
- Non-compliance (attitudinal) errors are of three types. Routine errors are deliberate deviations from the approved routine (“I like my way better.”). Situational errors take short cuts or improperly follow the procedure to save time or effort on a particular case (“I need to catch up with this surgeon now!”). Emergent cases are particularly susceptible to this error. Exceptional errors are well-meaning, but misguided routine procedural errors that occur repeatedly on many cases (“I am under pressure by my boss to always get the job done on time.”)
- Exacerbating factor errors are caused by such things as fatigue, stress, hunger and illness.
- Checklist design errors are caused by poor design, poor wording, being too short or too long.
Checklists are best executed using a verbal challenge and response format. Verbalize the task out loud, even if there is only one operator. Verbalizing the task helps to stimulate the thought process and block the autonomic response. Physically complete the task while repeating the task verbally before marking the item on the checklist. Avoid irrelevant distractions and interruptions when possible. Otherwise complete a specific checklist task before addressing the outside distraction. Ensure sufficient time to complete the checklist. And lastly, take a short “time out” before bypass initiation to confirm to the surgeon and everyone else in the room that the open heart pump is ready and safe to be used. Failure of the open heart pump to operate properly is not only risky for the patient, but it exposes everyone in the room to involvement in a potential litigation. The other cardiac surgery team members should be reassured that the pump is ready and safe to use. If time is short due to an emergency, there should be a space on the checklist to indicate that the case is “Emergent”. This would explain and justify any checklist non-conformance due to the urgent situation.
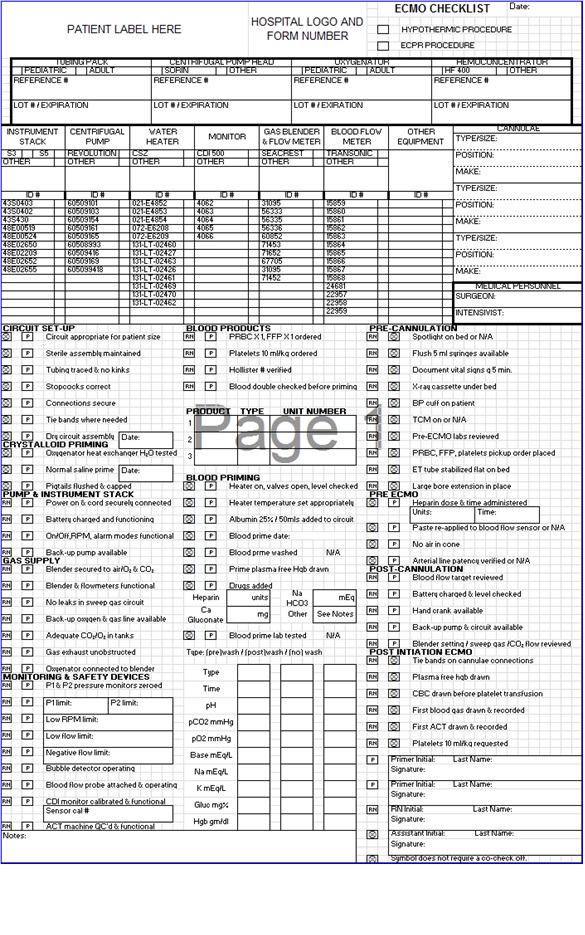
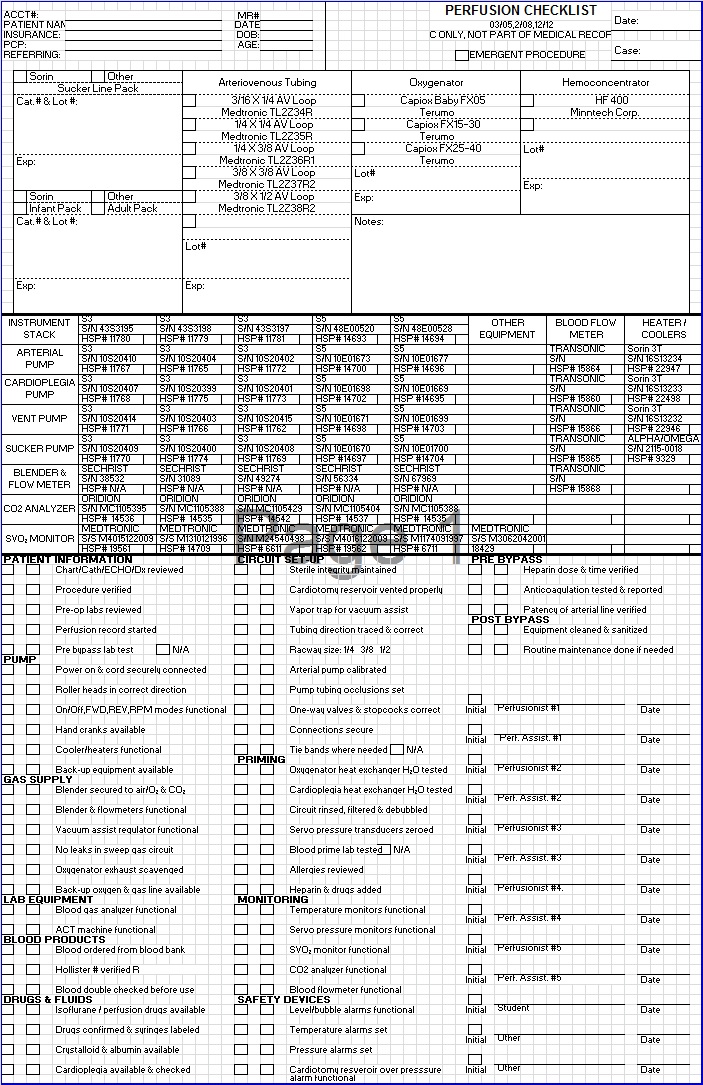
AmSECT Standard 3.2 indicates that the perfusion record should contain “Information sufficient to accurately describe the …. equipment.” The AmSECT Standards don’t specifically require it, but the description of important equipment and disposable supplies including serial and lot numbers should appear on the checklist if not on the perfusion record. Below are old hard copies of ECMO and CPB checklists I have used in the past. Most things are computerized now. But the content and comprehensiveness of these documents is still relevant.