Say “Hello” To ECMOjo !
Perfusion simulators for training are becoming very popular and a new Source Forge open source simulator called “ECMOjo” from Hawaii is now available to anyone wishing to test their skills in using a heart/lung machine in the form of an ECMO pump to keep a patient alive; http://ecmojo.sourceforge.net/. A tutorial and demonstration is on YouTube as well. The latest version of ECMOjo in English became available in September 2010. Japanese and Spanish versions are also available.
ECMOjo is not a typographical error; it is a contraction of two words, ECMO and mojo (a magical charm). The program was developed by the Telehealth Research Institute at the John A. Burns School of Medicine of the University of Hawaii, under a grant from the Department of Defense. The Hanuola Center uses this and other tools to train its physicians, nurses and other personnel in the basics of ECMO. The Hanuola Center is the ECMO Program of Hawaii, which serves to provide pediatric extracorporeal life support services for Hawaii and the Pacific Rim region. The simulator was developed in cooperation with Tripler Army Medical Center, Kapi’olani Medical Center for Women and Children, Kaiser Permanente of Hawaii, the University of Hawaii and the University of Pittsburgh Medical Center. The project manager is Mark T. Ogino, MD, Hanuola ECMO Medical Director. Among many other contributors are two perfusionists who participated in the simulator’s development; Kristen Costales, CCP, ECMO Perfusion Coordinator and Kent Kelly, CCP.
ECMOjo is an open source program, which means it is free to use on-line or for download under the terms of the Berkeley Software Distribution License. It is available for Windows, Macintosh, Linux and UNIX operating systems. The simulator uses a graphical interface, delightfully illustrated by artist Kaleiohu Lee.
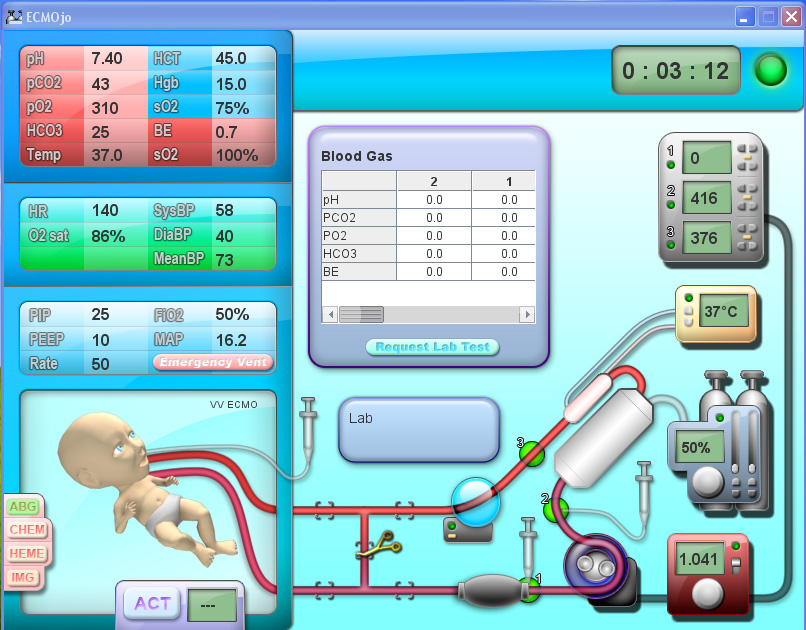
The ECMOjo screen is divided into left and right sides. On the left, the graphic interface shows a patient (an infant) attached by blood tubing to a heart/lung (ECMO) pump on the right side.
On the left side, the patient’s blood pressure, arterial blood saturation, heart rate, venous blood saturation, temperature, respiratory rate and other parameters are displayed above the patient. Modifications to the circuit cause changes to the patient values. For example, if the VA ECMO pump flow is increased, the patient’s blood pressure goes up. If the sweep gas flow is reduced, the patient’s pCO2 increases. If the water temperature is reduced the patient’s temperature goes down. If the pump stops altogether, the patient will rapidly decompensate in all vital areas. Lab values such as arterial blood gases, hematology (CBC & coags), electrolytes, lactate, and ACT values can be reviewed and new values obtained. These can also change with pump changes; for example, increasing acidosis and lactate values correlating to decreasing pump flow. Chest X-rays and head ultrasound images can be viewed and cardiac ECHO reports read. Ventilator parameters can be changed from rest settings to emergency settings. Another indicator shows if the patient is on venoarterial or venovenous ECMO.
Placing the cursor over the patient brings up a menu that allows the operator to suction the endotracheal tube, check the cannulae for bleeding or kinks, assess urine output, assess level of sedation and even check for a dirty diaper. A short summary of the patient’s diagnosis and current status can also be viewed. During the simulations, the patient status may worsen. This is visually enhanced as the patient becomes progressively paler and bluer. This visual change provides added urgency to each simulation.
On the right side of the screen is the ECMO circuit with its disposable components and hardware. The circuit can be checked or changed with the touch of a button. The pump flow can be regulated. The sweep gas FiO2 and flow can be controlled. The heater temperature can be changed or the unit replaced. The circuit pressure monitor alarm limits can be adjusted. There is a bubble detector and four interventional sites that allow the operator to administer PRBC, FFP, platelets, heparin, catecholamines, 5% albumin or sedatives.
On the top right is a timer/clock used during simulations to assess the operators speed at solving the various problems presented in the simulations. A red light flashes and an audible alarm sounds when the infant’s vital signs become abnormal. The audible alarm is unique and almost comical. It is reminiscent of the klaxon horns used in submarines (Dive! Dive! Dive!). Anyone in the room when the game is being played is inevitably drawn to see the cause of the strange noise.
On opening the program the operator can choose tutorials (Overview, Introduction, Detailed and Advanced) to train in its use. The operator can also choose to use venoarterial or venovenous cannulation, a silicone or hollow fiber oxygenator, and a roller or centrifugal pump. After gaining familiarity with the fundamentals, the operator can choose from two broad categories: Scenarios and Simulations.
Scenarios are step-by-step training exercises that teach the operator about the various procedures needed to deal with circuit and/or patient problems. These include such things as routine circuit checks, coming off pump and going on pump, pump failure, air in the arterial line, circuit failure, temperature control, sweep gas control, oxygenator rupture, high system pressures, etc.
Simulations are exercises to test the operator’s skill in recognizing a problem and correcting it. During the simulations a timer counts down to warn that some problem will soon develop. Once the counter reaches ‘zero’, another timer starts to measure the time needed for the operator to diagnose the problem and select the appropriate solution. For example, increasing system pressures might stop the pump, causing the infant’s blood pressure, heart rate and arterial O2 saturation to fall. The cause might be a kinked arterial cannula, which is corrected very simply. On the other hand, the high system pressure might be caused by a developing DIC which is clotting the oxygenator and which can only be detected by a review of the hematology labs and only corrected by changing out the entire circuit. If the cause of the infant’s deterioration cannot be readily determined, immediate resuscitation steps may be needed, such as infusing volume, giving catecholamines, or going to emergency ventilator settings. These may buy time until a solution can be found and the pump restarted. Other simulations might deal with equipment failure, progressive acidosis, platelet consumption, agitation, a large blood loss from an accidental arterial decannulation, or a number of other things. If the problem is diagnosed and solved before the allotted time expires, the patient survives. Otherwise, the patient expires and the operator fails the exercise.
ECMOjo is still a work in progress. There seem to be a few bugs in the system. But, the website has contact links to the Telehealth Research Institute and encourages feedback by users to help in solving these problems.
On first impression, ECMOjo seems like a quaint, fun, ECMO video game. But it is really much more sophisticated than it first appears. Even an operator with 40 years of perfusion experience and 25 years of ECMO experience (like me) can find this program quite challenging. So say “Hello” to ECMOjo and have some fun! You might even learn something along the way.