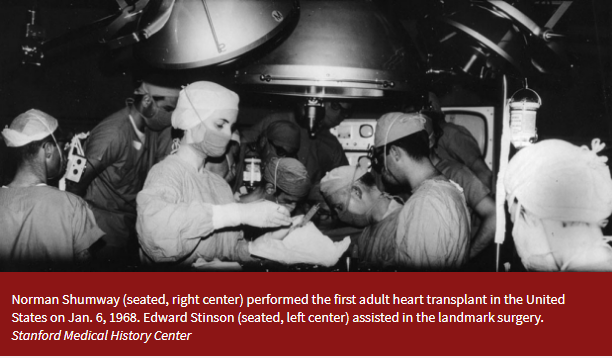
Part XVI- Norman E. Shumway And The Fruit of Curious Minds- Standing on Tall Shoulders- The History of Cardiac Surgery Thomas N Muziani PA-C, CP With An Ending Note By Mary Ann Overton CCP
“Success has many Fathers…but failure is an orphan” Italian Proverb and favorite quote of President John Fitzgerald Kennedy.
Einstein’s thought experiment- “What if?”
The day quickly approached when the first cardiac procedures were to commence at Children’s Hospital San Francisco. All the necessary equipment to conduct surgery was housed in the research laboratory. The only viable way to accomplish the move was to pack all their equipment from Stanford-Lane laboratories into a very large moving van and truck it to Children’s. The visual reminded some of the participants of the mass migrations to California during the Dust Bowl era. After the surgery…all of the equipment was packed up again, placed in the truck and transported back to Stanford-Lane.
The first case for Shumway and Cohn at Children’s was an atrial septal defect in a young woman performed under total-body hypothermia. Total body usually involved a very large rubber sheet placed under the patient. Once the patient was asleep, quite often with Ether anesthesia where you had to wear special non-conductive boots for fear of an explosion… buckets of ice were brought in and the patient was wrapped in a cocoon of rubber sheet and ice. If you were forced to lean in somehow against the patient, it would not take very long before your entire lower body would fall numb.
The early pioneers of cardiac surgery realized only too well there were several very distinct and mandatory aspects of the procedure that required constant vigilance to insure success. The first was utilizing extracorporeal circulation. The common analogy used at the time was trying to work on a busy thoroughfare, it mandated rerouting the traffic. You had to reroute the circulation to work inside the heart. Time works for and against you in cardiac surgery…it is one of the hallmarks to the yin and yang philosophy of this procedure: “You have to stop the heart to make it live?”
The second component was stopping the heart. The common analogy we used; “Imagine trying to sew an object constantly pulling away from you with thread as thin as a human hair”. However, stopping the heart and protecting the heart are two completely disparate concepts. Stopping the heart may temporarily lower the metabolic uptake but it in no way provides protection. Technically speaking, it’s very unnatural and immediately triggers the ischemic cascade. I am positive God intended to have the human heart stop just once. Shumway went looking for loopholes.
With the early acceptance and adoption of Denis Melrose’s technique in 1957 utilizing potassium citrate mixed in a liter of the patients own blood to arrest the heart, almost all cardiac surgeons felt they could check that hurdle off their list. The only problem was; potassium citrate is an extremely powerful poison and these early patients, as they like to say in South Texas: “up and died” rather quickly.
Denis Melrose was a very competent surgeon and felt if he could create an environment that would: “facilitate an unhurried repair”, he would insure success. Remembering the work of Sidney Ringer in London 1884, he believed that utilizing potassium citrate as the main arresting agent would be key. He loved the idea that everyone adopted its moniker of “Melrose Technic”. However, in 1958, McFarland performing post-mortem on these patients isolated citrate that produced citrate chelation as the main culprit leading to the deaths.
As a result in 1961, a consensus of cardiac surgeons imposed a moratorium of 15 years on the use of potassium based “cardioplegia”. In 1962, Dr. William L. Weirich wrote: “The use of the Melrose method of elective cardiac arrest induced by the single injection of a 2.5 percent potassium citrate-oxygenated blood solution has been abandoned by virtually all physicians who perform intracardiac operations.” (Prog. Cardiovasc. Dis. 4, 526–536., 1962).As a result, when I first started in 1968, we could only utilize intermittent cross clamp with fibrillation…a rather fascinating technique.
The third component of this triad was protecting the heart. This was by far the most elusive, comprehensively investigated and continuously debated…to this day.
Wilfred G. Bigelow, a former combat surgeon who grew up in the wilds of Manitoba and became Full Professor General Surgery at Toronto General in 1970 was a true pioneer, both in hypothermia and pacemaker development. In 1941 while serving overseas in the military as a battle surgeon during World War II, he observed the ravages of GI’s suffering from severe hypothermia. When he returned from service he studied at Johns Hopkins, Toronto General and University of Toronto investigating the effects of hypothermia. The concept of utilizing hypothermia during cardiac surgery has direct lineage to his voluminous articles and research on the subject. As a result Dr. Bigelow is considered the “Father of Hypothermia” and the utilization of his techniques are recognized as the first major breakthrough in protecting the heart during surgery. I am an unabashed fan of “Bill” Bigelow for many reasons and one of my favorite quotes from him is: “I always thought that patients never got enough credit for having courage”.
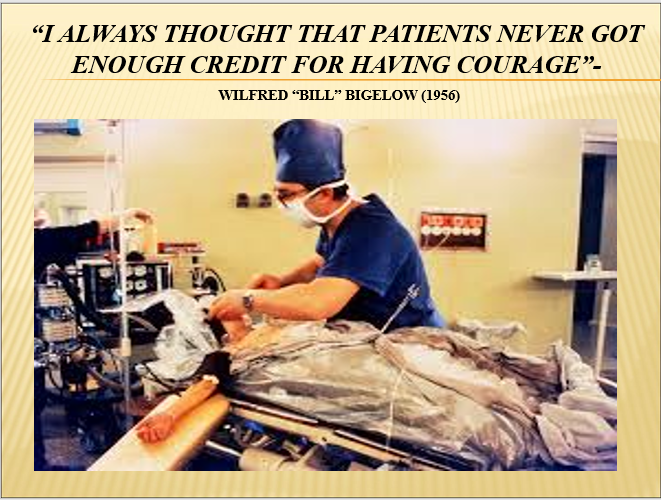
( Dr. Bigelow working on a total body hypothermia patient using ice and a rubber sheet coccoon.)
With all this information digested and dissected by Cohn and Shumway they realized their new program was essentially starting “with a clean sheet of paper” when it came to protecting the heart. Some procedures would be accomplished with the heart still beating and perfused, while others dictated greater accuracy in diagnosis, thereby necessitating “arresting” and creating a dry field. When the operation demanded they open the aorta which exposed the coronary arteries and denying them perfusion, they felt there were two methods to minimize the effects for onset of ischemia: A) use catheters and perfuse the coronaries or B) utilize potassium arrest. Neither technique was considered ideal. The first method cluttered the field, stopped the progress of surgery and was reliant on all sorts of mechanical complexity (e.g. proper insertion, ensured sealant of Spencer/Mallet cannulaes, kinked tubing) and the second method really gained no time and therefore was considered very dangerous if cavalier. Our gallows humor for potassium arrest was: “The surgery was a success but the patient died”.
Shumway approached this problem logically in the laboratory. Calling upon his hypothermia experience and the work that Bigelow had published, he realized total-body hypothermia created a very fine line between a viable beating heart and fibrillation. Once the heart feels 31 degrees centigrade it wants to fibrillate…and will not convert until it’s warm. However, if he utilized “topical hypothermia” there may be a window of controlling ischemia and accomplishing the necessary repair. In the dog lab he reduced the animal’s temperature to 32°C utilizing perfusion. Then, catheters were sutured around the edge of the opened pericardium which had been sutured to the edges of the sternal wound…creating a cradle. The cold saline was continuously circulated throughout the pericardial “cradle” and sucked out.
This allowed the aorta to be opened, necessary repair to commence, unclamping the aorta and blood flow restored. The heart was defibrillated and supported with bypass until the myocardium could easily eject and maintain a stable pressure on its own. Successful experiment after experiment was accomplished validating the utility of topical hypothermia as an integral modality for whatever cardiac surgery performed.
The experiments increased, the minutiae fine-tuned and arrest times became longer and longer. This waiting period allowed Shumway and colleagues to imagine what other methods they could incorporate to insure a positive outcome. There was no question that standing in one spot for extended periods of time was a major drain both physically and mentally. They discussed for hours “bench heart surgery” where the cooled heart was excised from the chest and operated on a figurative back bench…replacing broken parts and sewing defects under more controlled precise environment.
So, Dr Lower started experimenting with excising the dog heart and then suturing it back in. He utilized the same technique for excising the heart that he was trained for with postmortem examinations. This allowed for him to work on the heart with acute precision to accomplish a correction. Unfortunately, the procedure proved unsuccessful mainly due to the fragile nature of the experimental animal’s aorta. There was insufficient tissue to manipulate the heart in the canine model.
However, this experimentation provided validation and visions for saving thousands of lives plus profound exhilaration for the discovery of the “Holy Grail” of cardiac procedures…actually removing and replacing a broken heart with a viable fresh organ. A start-over.
As I used to exclaim once the patient was induced and chest opened: “Let’s make the Mayan’s proud!”