Dr, Mustard’s Macabre Monkey Machine by Gary Grist and Kelly Hedlund

Dr. William Thornton Mustard MD
Dr. William Thornton Mustard (1914 – 1987) was uniquely brilliant. At 22 years of age, he was the youngest physician in Canada in 1937. While serving in Europe during WWII, he performed limb salvage on soldiers by connecting severed arteries with glass tubes. In 1947, he joined the staff of the Hospital for Sick Children in Toronto and began practicing both general and orthopedic surgery. During this same time, he traveled to Baltimore to spend a month at Johns Hopkins University observing Dr. Alfred Blalock and Vivian Thomas where he learned to perform the Blalock-Tauusig shunt for ‘blue babies”. Upon his return, he became the de facto champion of congenital heart surgery in Toronto.
Hips and Hearts
In 1948, he did the first total blood replacement in a newborn with Rh incompatibility. In March 1949 Dr. Mustard and Dr. A. L. “Laurie” Chute performed the world’s first open-heart operation on a dog at the Banting Institute using their experimental heart lung machine. “We never did get a picture of that dog. We should have had one like Banting and Best of the first insulin dog. I think ours was the first dog in the world to survive having its heart opened.” Simultaneously, Dr. Mustard amassed a large series of coarctation repairs, patent ductus ligations, and Blalock shunt procedures in Tetralogy of Fallot patients. He also earned international recognition for a procedure for polio patients that would become known as the (first) Mustard procedure. Healthy iliopsoas muscle was moved from the front to the back of the hip to replace the hip abductor damaged by the virus. This enabled polio victims to walk normally without a disabling limp.
Wit And The Social Graces
WTM was also outrageous. In medical school he showed more interest in athletics (gymnastics) and theatrics (participating in the school show “Daffydil” where his wit and comic talent made him the star) than he did in his studies. When he learned that his wife was expecting twins he said, “The Americans split the atom but we split the ovum.” At parties he would swallow live goldfish for a laugh. If the occasion was formal, he might start a food fight or jump into a fountain wearing a tuxedo. He was the opposite of highbrow and loved being the unpredictable showman. When lecturing his students, he would sometimes stand on his head at the front of the class. A colleague of Mustard’s was quoted as saying, “Mustard is so skilled at surgery he can sew two farts together.” Yet, despite his proclivity towards humor, professionally, Dr. Mustard’s genius was unmistakable and serious.
“Wild Bill”
His colleagues affectionately called him “Wild Bill” – a nickname he earned because his daily routine often consisted of doing blue baby operations in the morning and club foot repairs in the afternoon. Of course, his best-known contribution to medicine was the intra-atrial baffle for Transposition of the Great Arteries (referred to as the second Mustard Procedure), which was first used on a three-month-old girl on January 17, 1952. The procedure was refined in the 1960s and brought him instant fame. For the next thirteen years (he retired in 1976) patients from all over the world sought him out for care. Lesser known was Mustard’s early attempt at building a workable heart-lung machine (see description below).
The Three Amigos
In the early 1950s, Dr. William Mustard MD, Dr. Andrew “Laurie” Chute MD of the University of Toronto Medical School, and Mr. Campbell Cowan of the Banting Institute developed a heart-lung machine that used isolated monkey lungs as the oxygenator. The work was funded by grants from the Banting Foundation. Dr. Mustard hoped to use human lungs initially, but a banking system for them was not yet developed. It was a sign of desperation at the time that rhesus monkey lungs were the best alternative. The “washed” Macaca Rhesus monkey lungs were considered clinically satisfactory.
Twenty Minute Lungs?
The monkeys were part of a renal study being conducted by the Connaught Medical Research Laboratories and were scheduled for euthanasia at the completion of the study. After the kidneys were removed, and while still anesthetized, their chests were shaved, prepped and draped. When the chests were open the monkeys were exsanguinated, and the hearts and lungs removed en bloc. The procedure was performed on four monkeys for each surgery. The lungs had to be used within 2-5 hours post mortem. Otherwise, edema would likely preclude their use. Four pairs were prepared so that if the first pair did not expand well or developed edema during the case, a replacement pair could be used. This raised the problem that replacement lungs were closer to the post mortem time limit and might not have functioned as well for as long as the first pair. According to The Banting Research Foundation Hall of Fame documentation, each set of lungs would only last about 20 minutes, so several were needed as backup. But in his 1954 article, Dr. Mustard claims that the monkey lung oxygenators lasted “2 to 4 hours before showing any deleterious effects.” So, the need for three backup lung sets seems an inconsistency in reviewing written resources.
Urgency Needed
The right atrium, right ventricle, and the left ventricle were excised with the left atrium left open. A cannula was placed in the trachea, which would be attached to a tube delivering oxygen to the lung pair. Another cannula was placed in the pulmonary artery for blood perfusion from a venous pump. The whole process was done with some urgency, and as soon as possible a cold solution of 6% dextran in normal saline containing 10 mg heparin/L, 400,000 units/L of penicillin, and 1000 mg/L streptomycin was flushed by gravity into the lungs’ vascular tree. Manual massage and visual inspection of the lungs ensured complete lung washout and blanching except where there were parasitic scars, which were present in about one-third of the lung sets. The lungs remained functional for only a few hours after this preparation.
Unique Circuit Design
The circuit design began with dual cannulation of the right atrium and gravity drainage to a venous reservoir (Fig. 1). The blood was then pumped from the reservoir up into the pulmonary artery of a pair of monkey lungs suspended in lung jars. These were positioned in the uppermost area of the machine so that the oxygenated and ventilated blood could again drain by gravity into an arterial reservoir. As the lungs were perfused, 100% oxygen flowed by a tube into the trachea by the previously described cannula. The lungs were ventilated by intermittent opening and closing of a relief port by a technician putting a finger on and off the port. This on-and-off motion had to be continually performed while the patient was on the pump. The blood drained from the open left atrium into the bottom of the lung jars where it was channeled into the arterial reservoir.
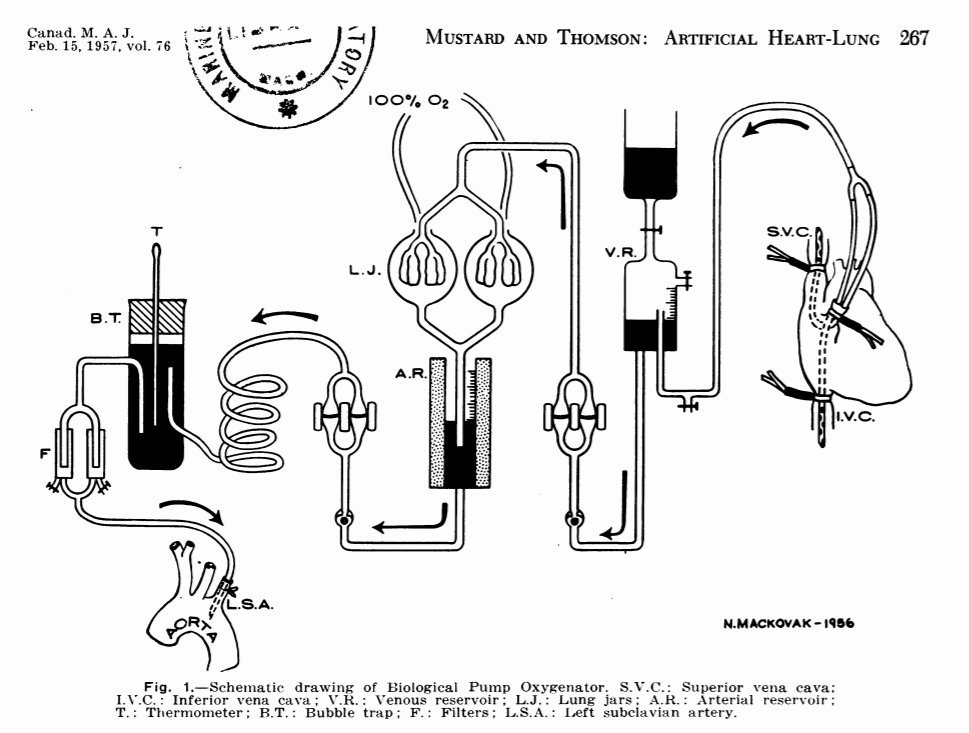
Figure 1
Bulbs And Cams
There were two pumps in the circuit: one pumping out of the venous reservoir to the lungs and the other pumping out of the arterial reservoir and into the patient’s left subclavian artery after passing through a coil heat exchanger, a bubble trap, and two filters. Each pump had two flexible bulbs with one-way directional valves. The two bulbs were positioned within a cam device that alternately squeezed one bulb while allowing the other to refill with blood. The cam device could be sped up to pump more blood or set to squeeze tighter or looser to change the stroke volume of blood pumped with each cam cycle. Hemolysis caused by the artificial surfaces and unnatural turbulence was a constant worry, but the average post-pump plasma hemoglobin was only 33 mg%. Figure 2 is a photograph that shows the machine with its cam system and only one lung jar. Part of the circuit can be seen. However, the venous reservoir, arterial reservoir, arterial bubble trap, and final filters are not seen.
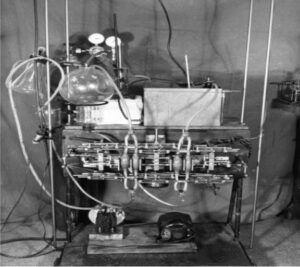
Figure 2
The Lungs In Action
This video shows the pumps in operation with a technician changing the speed and stroke volumes to balance the flow between the venous and arterial pumps. Another technician can be seen ventilating one pair of lungs by intermittently opening and closing the relief valve with his finger. A second lung pair can be seen in the second lung jar at the ready if needed. Hypothermia down to 25⁰C was used, and the heart was stopped for 3-5 minutes. Continuous oximetry was performed during bypass and arterial oxygen saturations down to 85% were acceptable unless pulmonary edema prevented adequate ventilation from occurring. These disembodied lungs hanging in large glass spheres above the pump give it an air of the macabre, especially with one set of lungs constantly pulsating and dripping blood. <https://perfusiontheory.com/wp-content/uploads/2021/09/Monkey-lung-perfusion.wmv>
Prime Speculation
No information could be found in any publications on the priming process in our review. But it is likely that the system was primed with a balanced salt solution to wet the surfaces and remove air. Then four to six units of fresh, whole, heparinized blood drawn from human volunteers the morning of the surgery, were used to displace the saline prime.
Lots Of Problems
Dr. Mustard and his team did extensive laboratory experimentation using dogs and dog lungs before attempting the first human cases. Even so, his first seven patients all died using monkey lungs as oxygenators. There were several reasons for this. He chose the most complex lesions such as arterial transposition and tricuspid atresia. There was no dog model to successfully practice these techniques before applying the surgical repairs clinically. Additional problems that became evident included poor myocardial protection, intraoperative air embolism, diagnostic errors, postoperative bleeding, and many other problems that are either prevented or easily mitigated using today’s methods. Dr. Mustard’s machine had no field suckers, no cardioplegia, no ventricular vent and was without many of the other devices and techniques we are accustomed to today. It is amazing that he had any survivors at all!
The Risk Philosophy
The philosophy at the time was that less risky patients should not undergo open heart surgery because of the extreme risk of using the pump. They had a chance, however small, of living past three years of age despite their congenital heart disease. Instead, the sickest patients were chosen and only those children who were not expected to live past two or three years of age would be operated upon, primarily for closure of ventricular septal defects, repair of tetralogy of Fallot or atrioventricular canals (AV communis). In 1957, Dr. Mustard reported on 21 more patients using the monkey lung machine with only three survivors (14% survival). Dr. Gibbon’s record of six patients (four reported, two unreported by him) with only one survivor (17% survival) before giving up is comparable. In the mid 1950’s, better pumps and artificial oxygenators became available. Dr. Mustard realized that monkey lungs and cam operated bulb pumps were dead-end technologies. So, he continued on with the newer technology even though past survival had been dismal. He never gave up hope of achieving successful palliative treatments for congenital heart disease.
A Personal Perspective
Bill Williams (William Galbraith Williams, M.D. gg), who is the retired ex-chief from Toronto and who knew Bill Mustard well forwarded this lovely message for this article:
“Yes, he was an orthopedic surgeon first. Because there was no cardiac surgery to speak of in 1947. But after a few years, the chief of surgery at SickKids asked that someone figure out what this new specialty of cardiac surgery was all about. Mustard volunteered and went to Johns Hopkins for 6 weeks to watch Blalock (coached by Vivian Thomas) do a Blalock shunt each morning. On his return to Toronto, John Keith (a cardiologist. gg) asked him to operate on a child with a PDA; then a child with a coarctation – each of which he did by reading case reports, never having seen either. That prompted him to ask Keith if he ever saw any blue babies?
“Mustard continued to do a little orthopedics. When I was his resident, he’d have me find out what the chief of orthopedics, Bob Salter, had booked, then book the same operation for Mustard. He then made great fun of showing up in Bob Salter’s OR to ask how his operation was going and telling him, “My patient is already awake in the recovery room”.
“Mustard also told the story of giving a cardiac paper in Mexico City. After the lecture, an orthopedic surgeon spoke to him to say that he didn’t understand much of the lecture but wanted to say hello to Mustard because he did his father’s ilio-tendon transfer operation. (Bill’s father was a school teacher)
“Mustard was a champion diver in his youth, a gymnast and was known to walk into a lecture hall on his hands to get a the medical class’ attention. He was loved by the staff, a very gentle humble man and was intent on ridding the world of arrogance. And THE most honest person I’ve ever known. A truly unique and wonderful man!”
