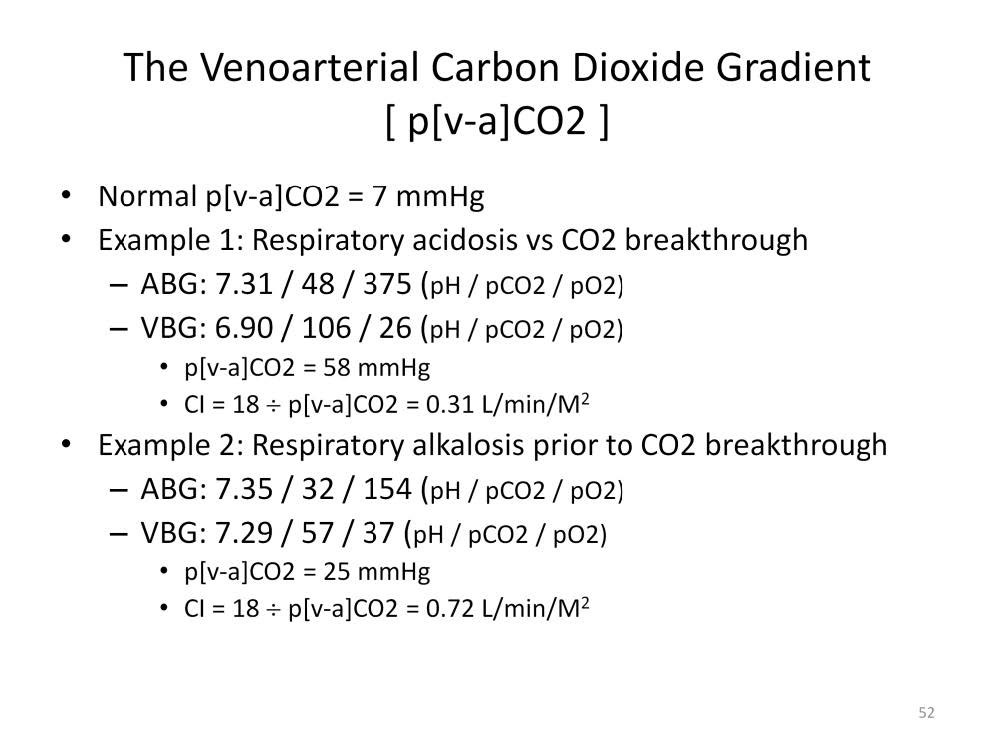
The magnitude of the accumulation of CO2 within the tissues can be masked in the patient unless both arterial and venous blood gases are measured at the same time. In a real life example, an arterial blood gas, 7.31 / 48 / 375 (pH / pCO2 / pO2), is diagnosed as a mild respiratory acidosis. This interpretation would normally prompt an increase in the ventilator rate and/or airway pressure which tends to impair cardiac function. A venous blood gas drawn at the same time was 6.90 / 106 / 26. The venoarterial CO2 gradient was shown to be a colossal 58 mmHg. An elevated venoarterial CO2 gradient is associated with sub-optimal cardiac function and poor perfused capillary density. Increasing the ventilator rate or airway pressure in an ill conceived attempt to reduce the paCO2 would further impair cardiac function and hasten this patient’s demise. This particular patient died from a large brain hemorrhage within 24 hours of being placed on ECMO. Contrary to the interpretation from the arterial blood gas, this patient did not have respiratory acidosis in the true sense that CO2 was being retained at the pulmonary level. In fact, the lungs were working extremely well to reduce the pCO2 from 106 to 48 mmHg and to increase the pO2 from 27 to 375 mmHg. What was diagnosed as arterial hypercapnea was in reality ‘CO2 breakthrough’ to the arterial blood due to the overwhelming inflow of CO2 into the lungs by the venous blood. This indicates severe cardiac dysfunction and poor perfused capillary density resulting in a lethal intracellular acidosis caused by CO2 accumulating in the tissues.
A second example illustrates how the arterial blood gas may appear hypocapnic while the venous blood gas is hypercapnic simultaneously. The arterial blood gas is 7.35 / 32 / 154 which can be interpreted as a mild metabolic acidosis with respiratory compensation. However, the venous blood gas is 7.29 / 57 / 37. There is no ‘CO2 breakthrough’ yet, even though the venous CO2 is elevated. But the venoarterial CO2 gradient is 25 mmHg, much higher than the normal 7 mmHg. So if only the arterial blood gases were examined, there would be no laboratory confirmation that the patient’s cardiac function is sub-optimal and that tissue acidosis is critical. This patient also died of a large brain hemorrhage.
According to the Krogh model, the venoarterial CO2 gradient can be used to assess the global degree of intracellular trapping of CO2. The mortality rate will increase as the venoarterial CO2 gradient increases until a point is reached beyond which no patient can survive.

Perfusion Theory is an educational platform for the Oxygen Pressure Field Theory (OPFT). August Krogh’s theoretical concept of the oxygen pressure field is explained and then applied to clinical applications in perfusion practice.